Take control
of your gut health.
Get in touch or apply for a test to get tailored recommendations and start getting on top of your gut health.
This is your gateway to an accurate diagnosis and a clear action plan from our trusted team of experts.
DIAGNOSTIC TESTS ACCREDITED & REGULATED BY

The UKAS Medical accreditation is for our clinics in London and Manchester

You deserve to get the diagnosis you need for better digestive health.
For too long, people have been living with unresolved gut issues and waiting years for a diagnosis.
We’re here to give you accurate answers, fast.
Get diagnostic testing and solutions actually backed by science, delivering the clarity you need at the highest standards.
Your path to better gut health starts here.


Get advanced diagnostic tests.
Our expert diagnostic services reveal what’s really happening in your gut, helping you find the right pathway to relief and better health.
At-home test kits
In-clinic test appointments
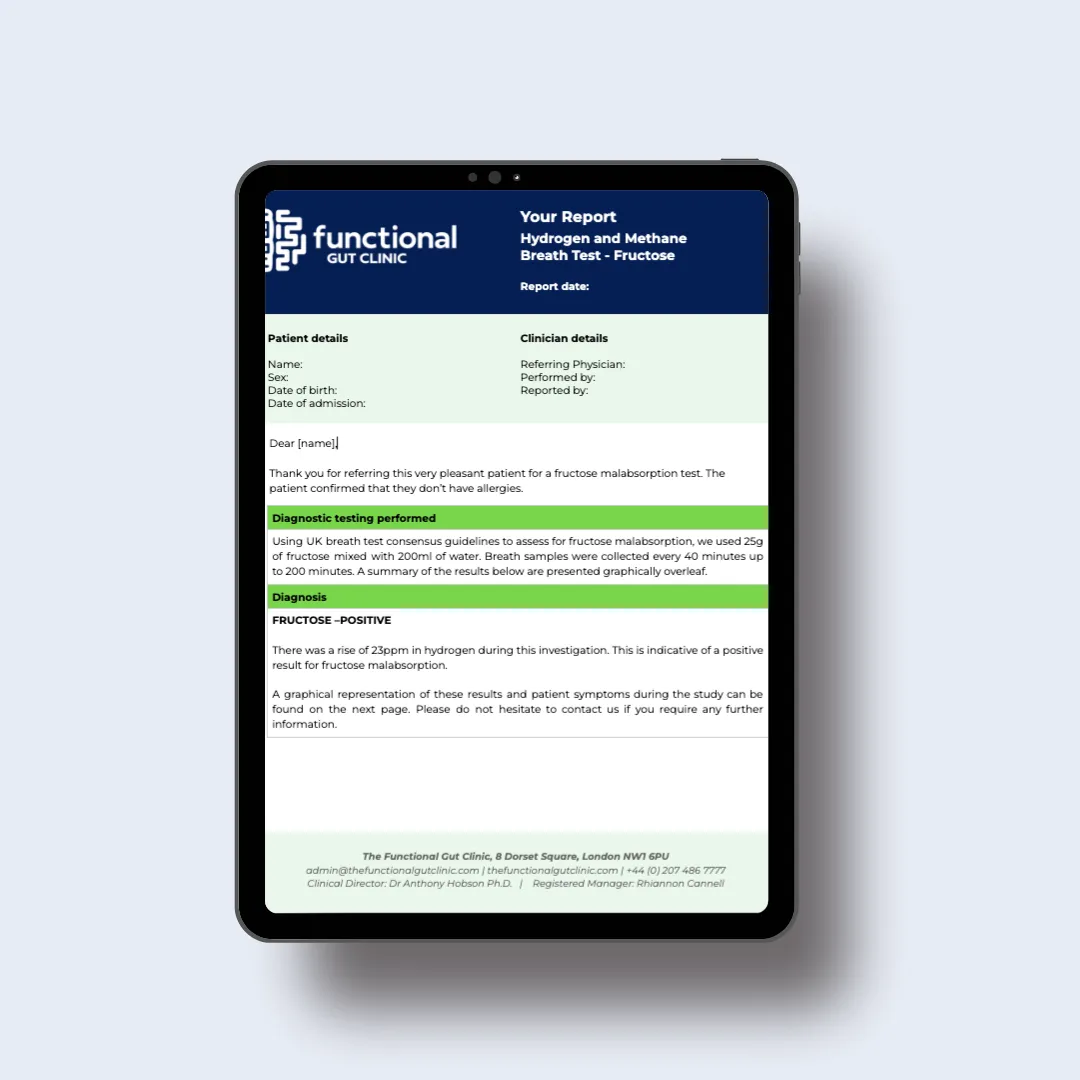
Detailed report written by our gut specialist clinicians
Our tests are fully regulated and accredited by:

The UKAS Medical accreditation is for our Functional Gut London Clinic only
Our Diagnostic Tests
Not sure where to start?
Take our 5-minute gut health questionnaire
Our guided self-assessment tool asks you some simple questions to find out more about your symptoms, so we can share personalised recommendations for the most suitable diagnostic tests for you.
How our testing works
Take our self-assessment or fill in our online booking form.
Simply share your symptoms, health history and goals on our online questionnaire - and we’ll analyse your data to give you our tailored recommendations.
Alternatively, if you already know what test you're looking for, complete our self-referral form to book your test.
(If you’re already under the care of another healthcare professional, they can also refer you to us.)
Order your at-home testing kit or book an appointment at one of our clinics.
Depending on the test, you’ll receive your at-home kit within 2-3 days, or you’ll be sent a link to book an appointment at your nearest clinic.

Get your results and report from your clinician.
Within 1-2 weeks, you’ll receive your test results, along with a detailed report from one of our clinicians with personalised recommendations - from treatment options to referrals to our fully vetted and trusted partners.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Your gut health is our priority.
Learn more about your symptoms, so you can get the best diagnostic tests tailored to your needs.
Reflux
IBS
Bloating
Abdominal Pain
Swallowing Issues
Diarrhoea
Incontinence
Constipation
Leading gut health specialists here to help you.
At The Functional Gut Clinic, we're a team of gut health specialists combining cutting-edge diagnostics with compassionate care.
Award-Winning Expertise: Trusted leaders in gut health.
Regulated & Trusted: Fully compliant with the highest standards.
Advanced Diagnostic Technology: Delivering accurate and reliable results.
Personalized Care: Tailored solutions for lasting symptom management.
Led by Prof. Anthony Hobson, our team of specialists is here to support your journey to better digestive health.
Learn more about our founder's passion and expertise that drives everything we do - and meet the people committed to transforming your health:

You’ve got your diagnosis. What next?
We're more than just diagnostic testing.
We provide a range of intervention and management strategies to help you get your gut back on track.

PelviPower
An innovative way to strengthen your pelvic floor. PelviPower can help improve bladder and bowel control, post-natal recovery and more.

Biofeedback
A comprehensive approach to bowel retraining, combining exercises, dietary advice and visual muscle feedback to treat constipation and incontinence.

Pelvic Floor Physiotherapy
Specialised physiotherapy to improve bowel movements, reduce pelvic pain and address dysfunction with tailored techniques.

PTNS Therapy
Advanced treatment using gentle nerve stimulation to improve bladder and bowel control.

Holistic Advice
Comprehensive dietary and lifestyle guidance to support lasting gut health and overall wellbeing.
Take part in our research
We’re driving developments in digestive health with innovative studies that will shape the future of care. This is your opportunity to put products and treatments to the test.
Join us and get involved in our research that’s transforming gut health.
