Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

Achalasia: A Symptom of Regurgitation
Achalasia is a swallowing condition where the lower esophageal sphincter (LES) that connects your stomach to your esophagus fails to relax. This prevents food and liquids from entering the stomach. It can cause difficulty swallowing, regurgitation, vomiting and chest discomfort.
Achalasia is a relatively rare condition. It’s often mistaken for other related disorders, such as gastroesophageal reflux disease (GERD). However, where GERD involves food coming from the stomach into the esophagus, achalasia prevents the food from ever reaching the stomach.
But what exactly causes achalasia? How is it defined? And what symptoms should you watch out for?
Find the answers below — and if you’re looking for expert care, visit us at The Functional Gut Clinic to learn more about our advanced diagnostic tests for achalasia.
What Is Achalasia?
Achalasia is the medical term for a condition where the lower esophageal sphincter (LES) fails to open during swallowing. Usually, the LES – a muscular ring of tissue separating the stomach and esophagus – acts like a valve, allowing food to enter but preventing it from leaving.
There are three main types of achalasia:
Type I (Classic Achalasia): Here, there is no evidence of muscle contractions in the esophagus together with no normal relaxation of the LES
Type II (Pan-esophageal): Here, there are no normal contractions of the esophagus. Instead, simultaneous contractions along the entire length of the esophagus occur together with no normal LES relaxation.
Type III (Spastic): Here, there is evidence of pre-mature or high-pressure, uncoordinated contractions in the lower esophagus occur together with no normal relaxation of the LES.
If the LES doesn’t relax, food begins to back up. This can cause problems with swallowing, leading toregurgitation.
The condition isn’t structural. Damaged nerves prevent the muscles of the LES from functioning normally, resulting in little to no relaxation.
Symptoms of Achalasia
Achalasia is a progressive condition. It starts mild and gradually gets worse over time. Common symptoms of achalasia include:
Difficulty swallowing (dysphagia)
Food or liquid coming back up (regurgitation)
Chest pain or discomfort
Heartburn-like symptoms
Unintentional weight loss
Coughing or choking, especially at night
A sensation of food sticking in the chest
Continually regurgitating food isn’t just unpleasant – it can presents serious risks such as aspiration pneumonia. This can happen if the food moves down the windpipe into the lungs. This severe version of the condition is difficult to treat with conventional antibiotics. People can also choke on the food during regurgitation.
Gastroesophageal reflux disease (GERD) or acid reflux can also cause similar symptoms. However, this condition is due to a weakened LES – the opposite of achalasia. It’s important to differentiate between these conditions as the treatments are not the same.
What Causes Achalasia?
The underlying cause of achalasia is poorly understood.
Researchers know that it involves the nerves that control the LES becoming damaged or dysfunctional. However, the exact mechanism by which this happens is unknown.
Potential causes include:
Genetics or family history – people with a close relative with achalasia are more likely to develop the condition.
An autoimmune condition – one theory is that the body’s immune cells attack the esophageal nerves, causing achalasia.
Physical damage – direct, traumatic damage to the nerves in your esophagus or LES will cause the same symptoms and condition.
Several infectious causes have also been suggested. Viral infections often precede autoimmune responses, especially in individuals with a genetic risk for the condition. Chagas disease – a rare parasitic infection – may be responsible for some cases in people living in Mexico, Central America, and South America.
Diagnosing Achalasia
Achalasia is often overlooked due to the similar presentation of GERD. However, it’s a relatively simple condition to diagnose. Your doctor may recommend:
Endoscopy – a thin, flexible tube with a camera on the end is passed into the esophagus. The physician can visualize the tube, looking for any signs of contraction. The test isn’t always diagnostic – it only leads to a diagnosis in around a third of cases.
X-ray – if an X-ray is performed, the test you will most likely perform is called a barium swallow. Here you consume a paste containing barium which is easily spotted on the X-ray, allowing doctors to see the outline of the esophagus. It produces the characteristic bird’s beak sign – due to the tapering of the esophagus resembling a bird’s beak.
Esophageal manometry – this test measures how the esophageal muscles work when you swallow. It detects pressure changes, which can rise if the LES fails to open. This test can also directly measure the LES, providing a definitive diagnosis of the condition as well as the type.
Esophageal manometry is the most reliable diagnostic tool. Some research indicates it’s accurate in diagnosing achalasia in more than 90% of cases.
Treatment of Achalasia
Achalasia cannot be cured. Once the nerves are damaged, the effects are permanent. However, depending on the type of achalasia you are diagnosed with, it can determine the success of treatments. For example, Type II achalasia has the best treatment outcomes.
Treatment involves widening or relaxing the LES to allow food and liquids to pass into the stomach. These treatments include:
Pneumatic dilation – an endoscope is passed into the esophagus alongside a special balloon. The balloon is inflated in the LES to stretch the muscle open. It carries some risks and can increase the potential for GERD.
Botox injections – Botox (or botulinum toxin) blocks the nerves signaling your LES to contract, allowing it to relax and let food pass through.
Laparoscopic Heller’s Myotomy – the LES muscle fibers are cut laparoscopically to help them relax.
Certain medications, including nitrates, calcium channel blockers, and sildenafil, are also given if surgery is not possible.
If you’re experiencing ongoing regurgitation, difficulty swallowing, or any of the symptoms above, visit us at The Functional Gut Clinic for expert testing and personalized care.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

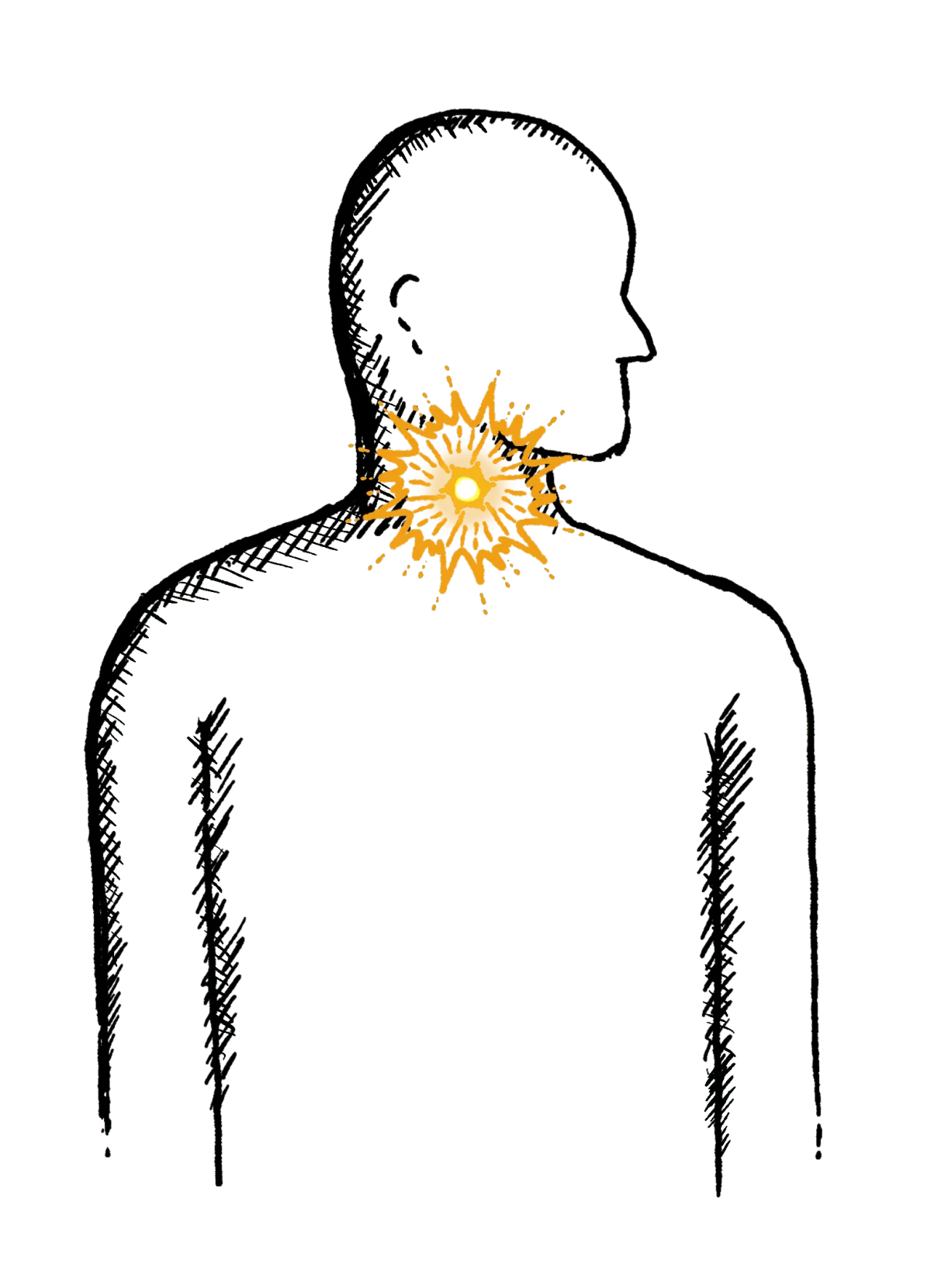
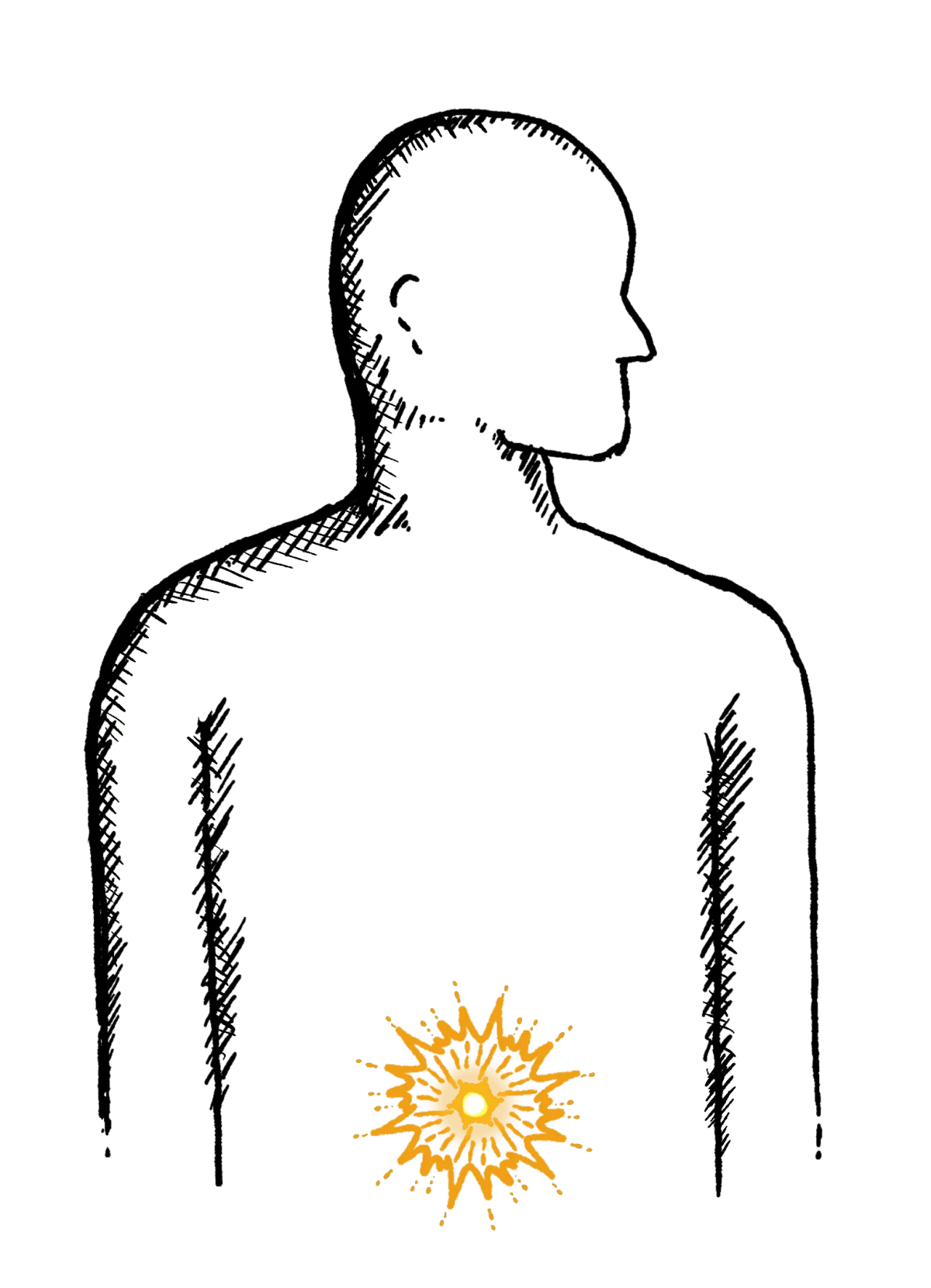
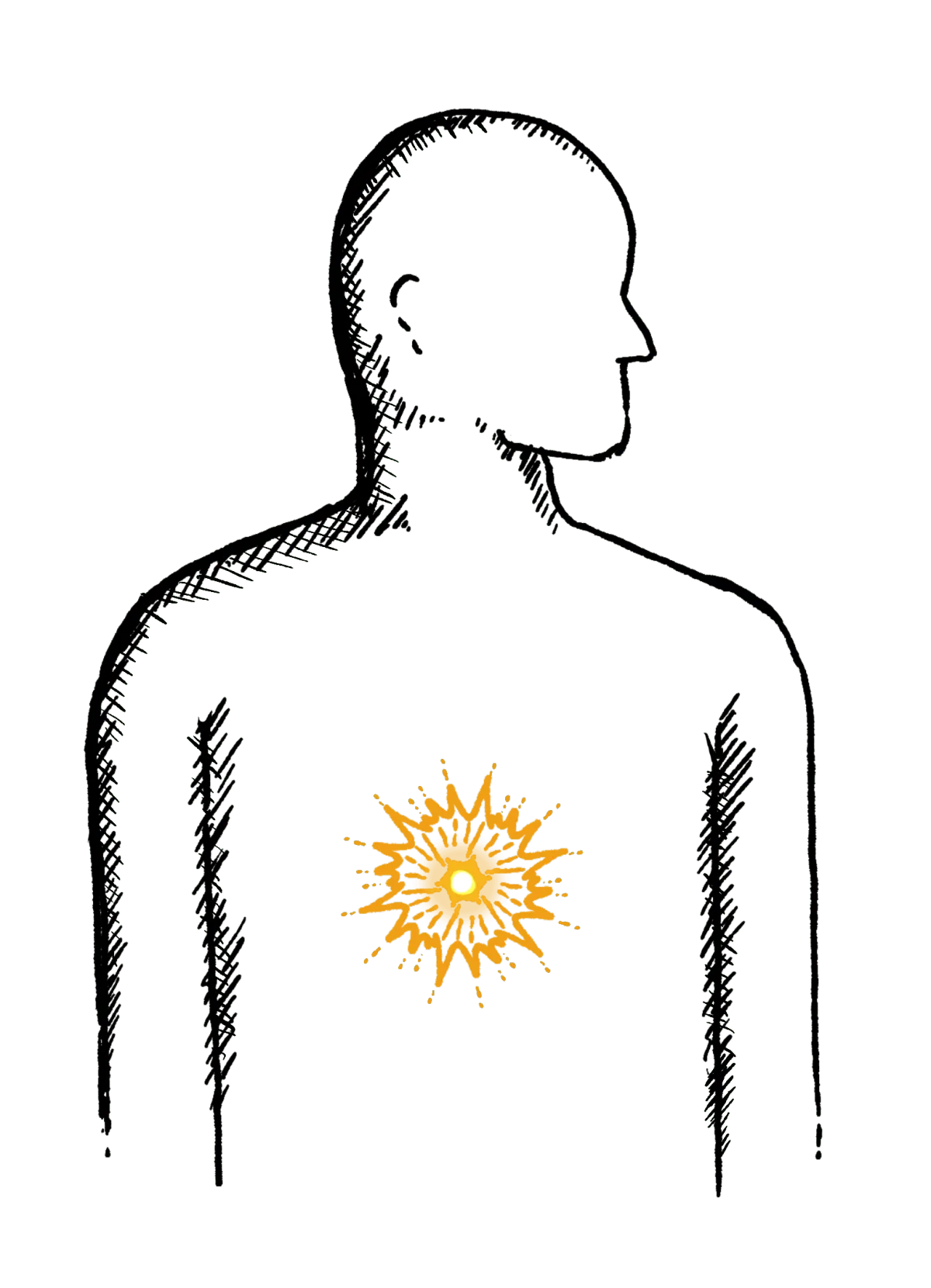
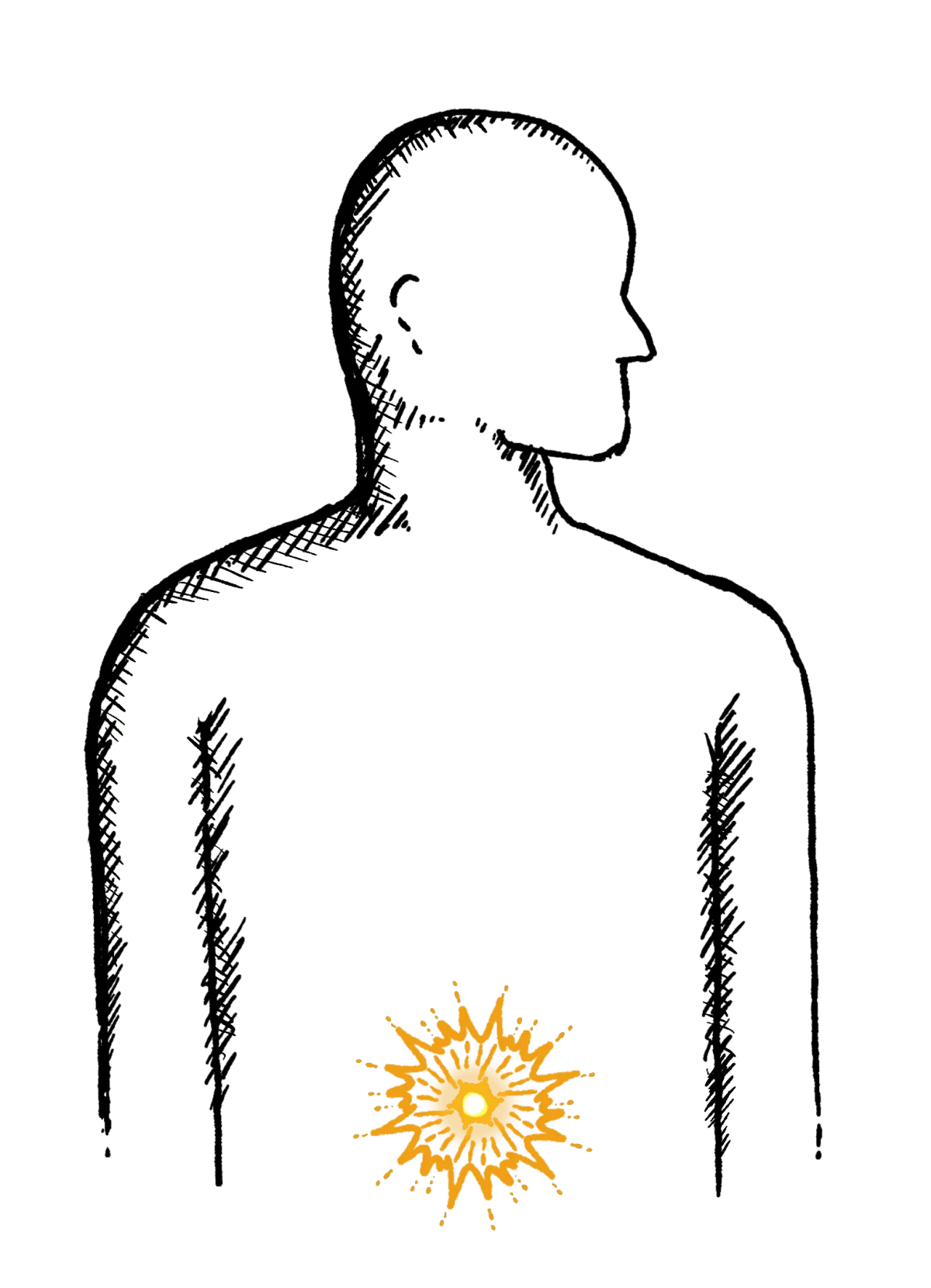
Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
Reflux
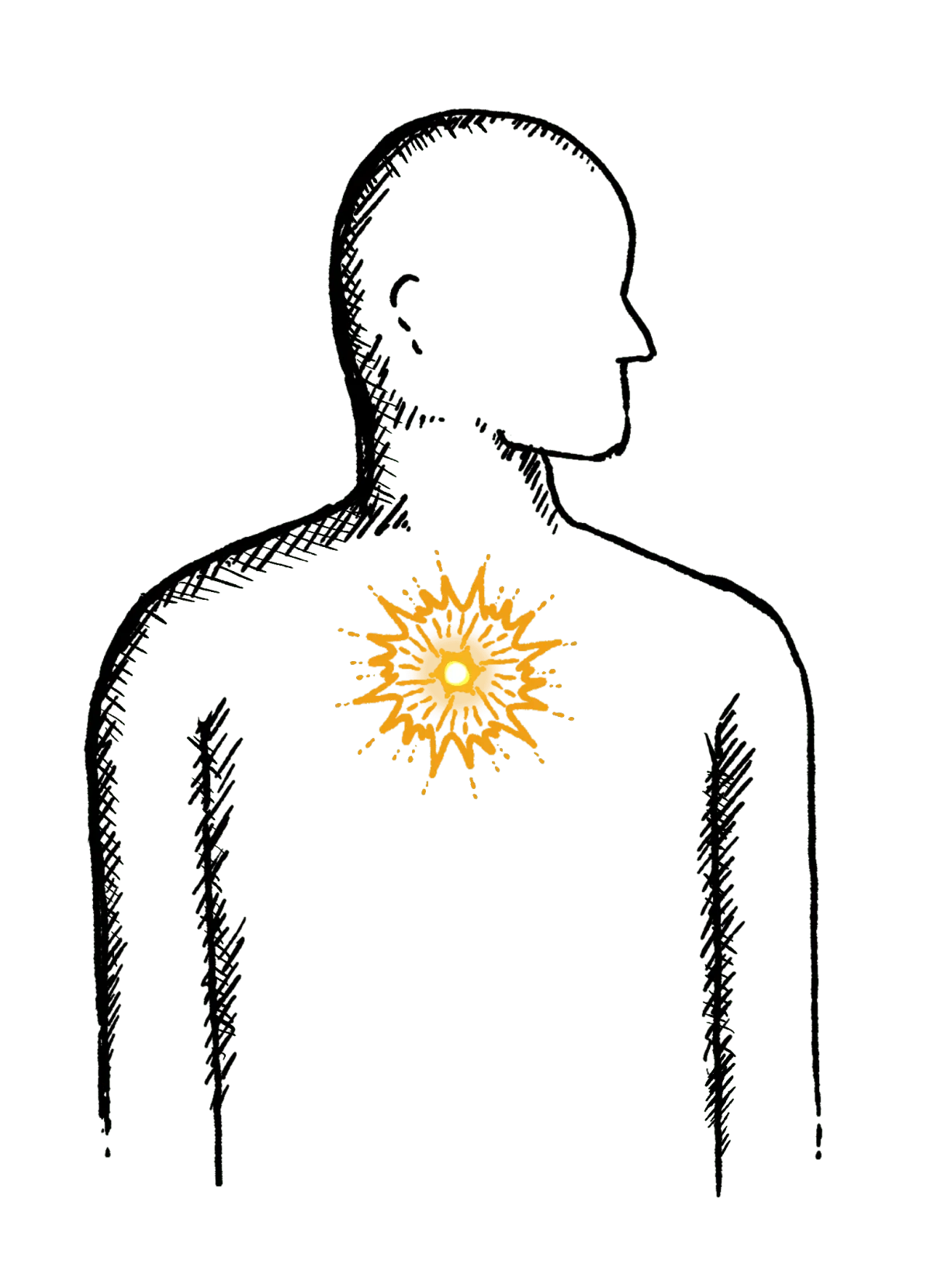
Burning mid-chest, worse when bending or lying down
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
Heartburn
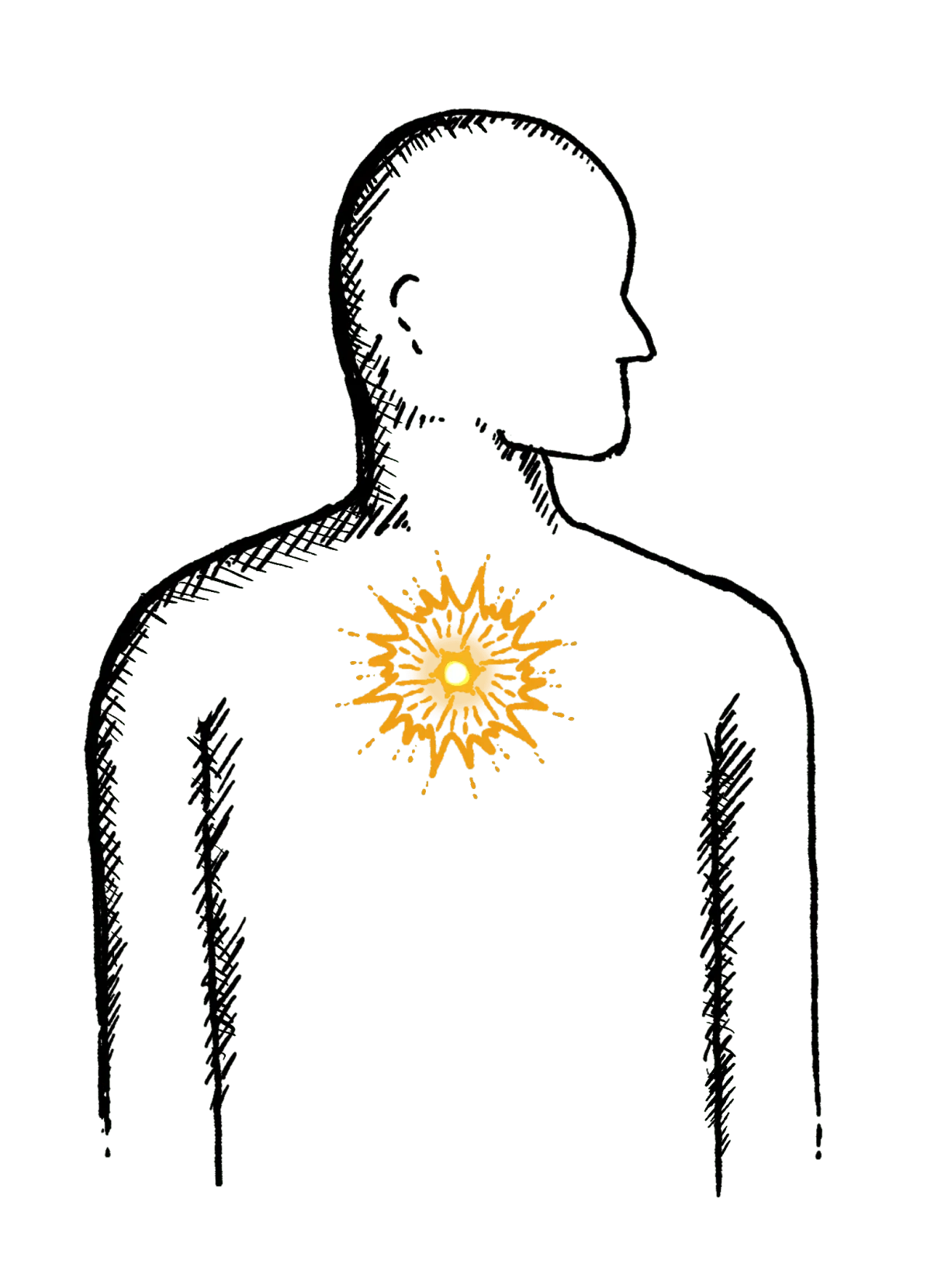
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
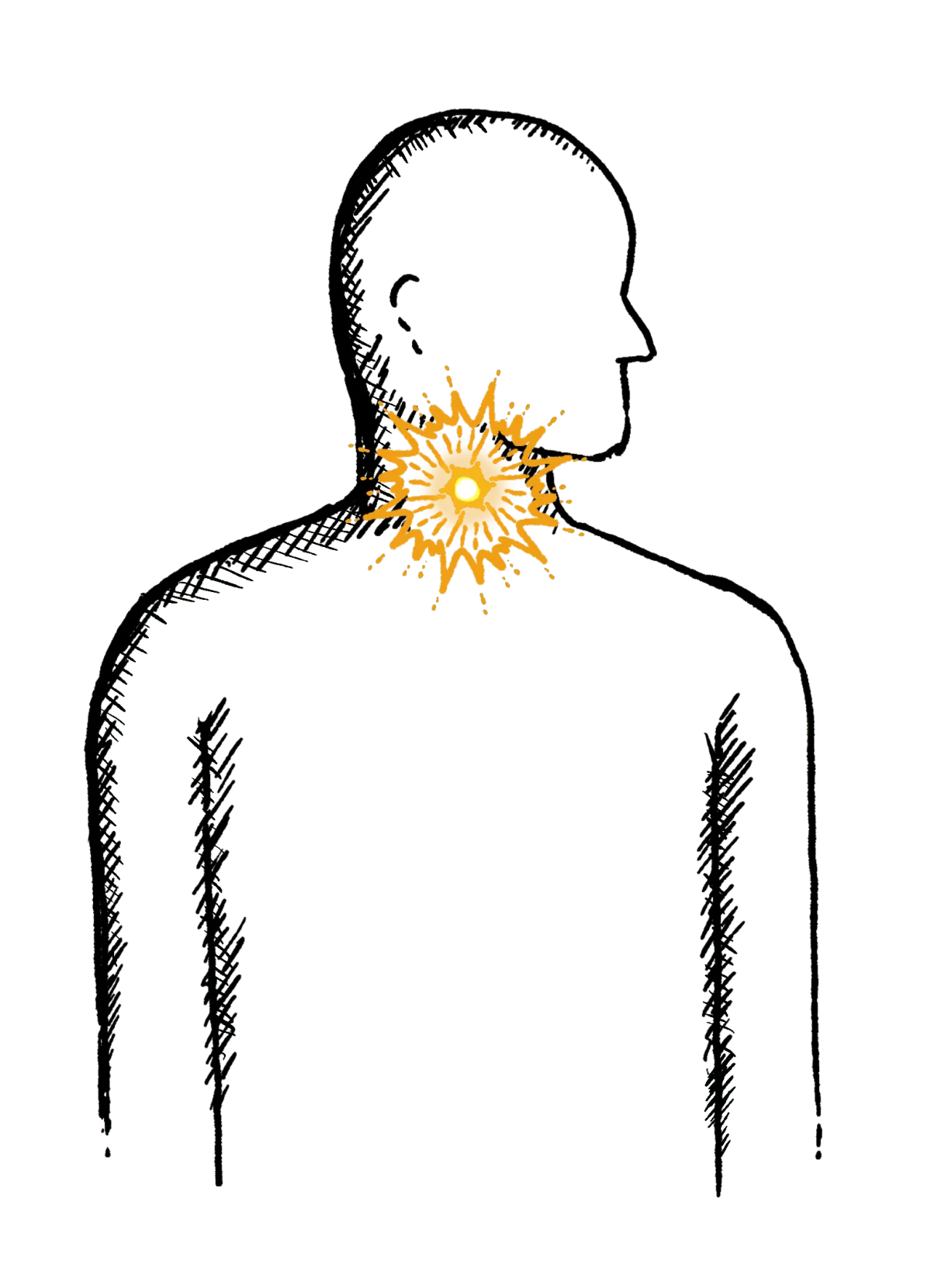
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Diarrhoea
Loose or explosive stools, can’t get to a toilet in time
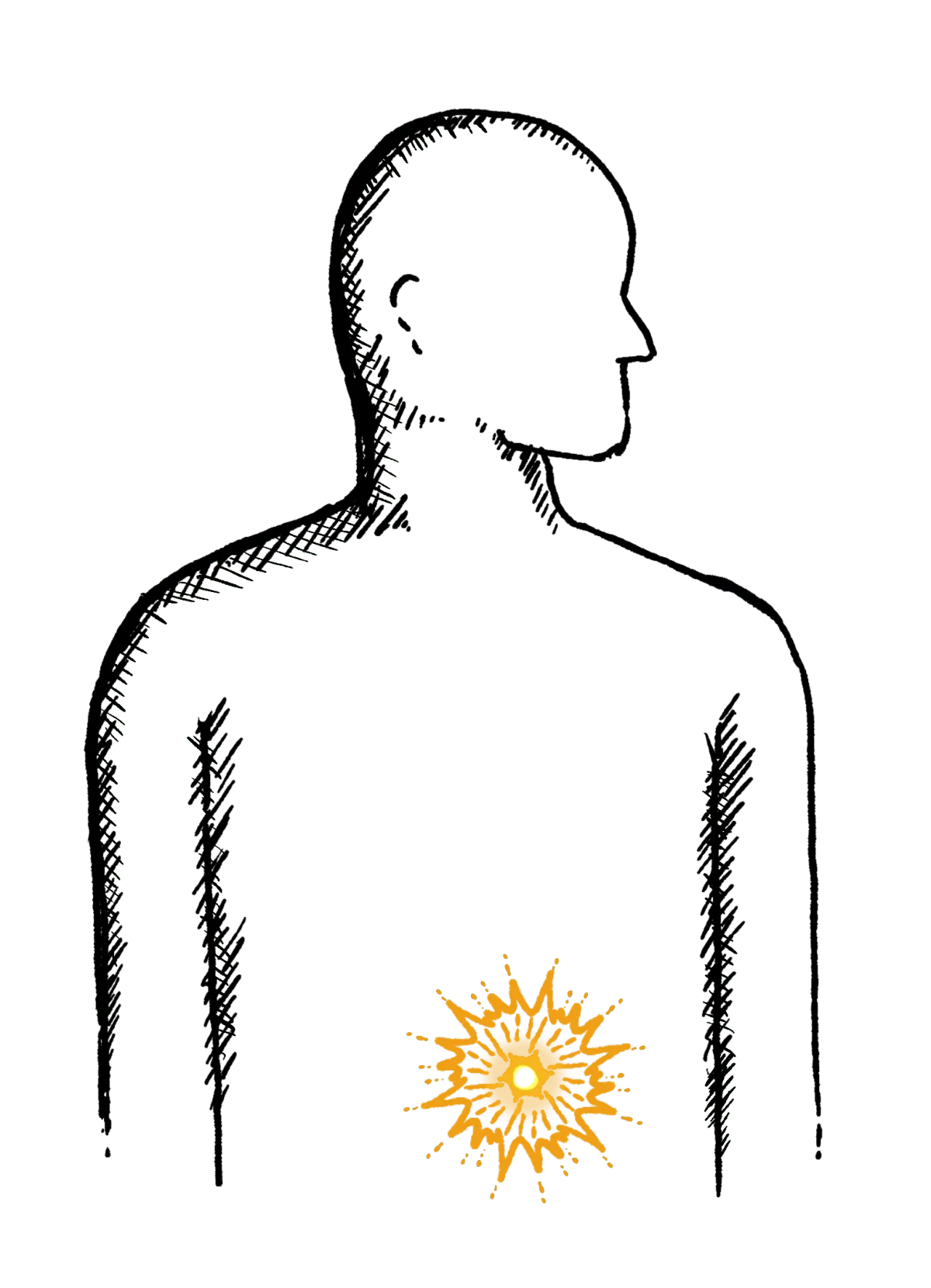
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

