Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

How to Improve Your Sleep When You Have GERD
Ever woken up in the night with severe heartburn? You’re not alone. Anyone who struggles with gastroesophageal reflux disease (GERD) knows that symptoms are often worse at night. It can be a major issue if it persists, causing tiredness, fatigue, and even emotional problems.
GERD is a chronic condition that occurs because acid from the stomach moves backwards into the oesophagus. This causes irritation, inflammation, and other symptoms, including poor sleep. But it doesn’t have to be this way.
So, if you’re wondering how to sleep better with GERD, we’ve got the solutions. Below, we cover the best tips to reduce GERD symptoms at night.
Don’t Eat Before Bed
Your stomach’s acid production is triggered by eating food. The more food you eat, the more acid you produce. Eating 2-3 hours before bed significantly increases your risk of heartburn and acid reflux.
One of the most common questions is the connection between acid reflux and sleep. It’s simple. Lying down in bed after eating allows the acid to pass into the oesophagus easily because gravity isn’t there to help keep it down. That’s why people notice an extreme burning sensation.
If you avoid eating for several hours before bed, you allow the food to exit your stomach, reducing the acid production, and so your GERD symptoms. You can also consider:
Going for a short walk outside
Doing some simple chores
Reading a book
Performing these tasks after eating gives your digestive system time to process the last meal. It’ll also help you get a better quality of sleep.
Prop Yourself Up with Pillows
If the primary issue causing acid reflux is lying down, there’s an obvious solution: sleep on an incline. Most people invest in some big pillows that allow themselves to sleep at a 45° angle or higher.
You don’t have to use pillows. Many GERD patients use a sleep wedge. This is a wedge-shaped pillow that keeps you partially upright during the night. According to the research, a sleep wedge between 8 and 22 cm in height is perfect for preventing GERD symptoms.
Another option is to put your entire bed on an incline. You can put bed blocks under the legs of your bed to raise one end. You want to ensure your head is higher than your feet.
Change Your Diet
Diet is one of the biggest triggers for GERD symptoms. Certain foods increase stomach acid production or relax your lower oesophageal sphincter (LOS), increasing the risk of GERD. These foods include:
Fatty or fried foods
Spicy foods
Chocolate
Citrus fruits (e.g., oranges, lemons)
Tomatoes and tomato-based sauces
Garlic and onions
Peppermint
Caffeinated drinks (e.g., coffee, tea, cola)
Carbonated beverages
Alcohol
Minimising consumption of these foods will alleviate your GERD symptoms. Another tip to stop acid reflux at night is to prioritise whole foods, e.g., lean proteins, low-fat dairy, and whole grains. These foods fill your stomach, reduce acid consumption, and support healthy sleep.
But it’s not just your diet. If you’re overweight or obese, it can contribute to your symptoms. Losing weight plays a critical role in improving GERD and ensuring you get the best night’s sleep possible.
Sleep on Your Left Side
Did you know the side you sleep on influences your GERD symptoms at night? That’s right. A 2023 review found that people who sleep on their right-hand side experience greater heartburn. This occurs because the stomach is higher than the oesophagus if you sleep on your right side, delaying gastric emptying and increasing backflow.
In contrast, sleeping on your left side can reduce oesophageal acid exposure by up to 71%. So, try sleeping in a different position if you struggle with nighttime symptoms.
Take Medication
If GERD symptoms persist no matter what you do, you may benefit from medication. During a GERD attack, always take an antacid. This will neutralise the acid, allowing you to get a good night’s sleep. However, antacids will not provide long-term relief.
Speak to your doctor about taking proton pump inhibitors (PPIs) or H2 blockers to reduce acid production. This should completely eliminate all GERD symptoms.
Learn More About Acid Reflux
Acid reflux doesn’t have to be forever. With the right lifestyle changes, medication, or other interventions, you can minimise your symptoms or eliminate them entirely.
Ultimately, the best tip to reduce GERD symptoms at night is to get tested and treated. The Functional Gut Clinic has developed a comprehensive guide to GERD and acid reflux symptoms, detailing the causes, tests, and treatments. We offer diagnostic testing for acid reflux, helping patients take control of their health.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
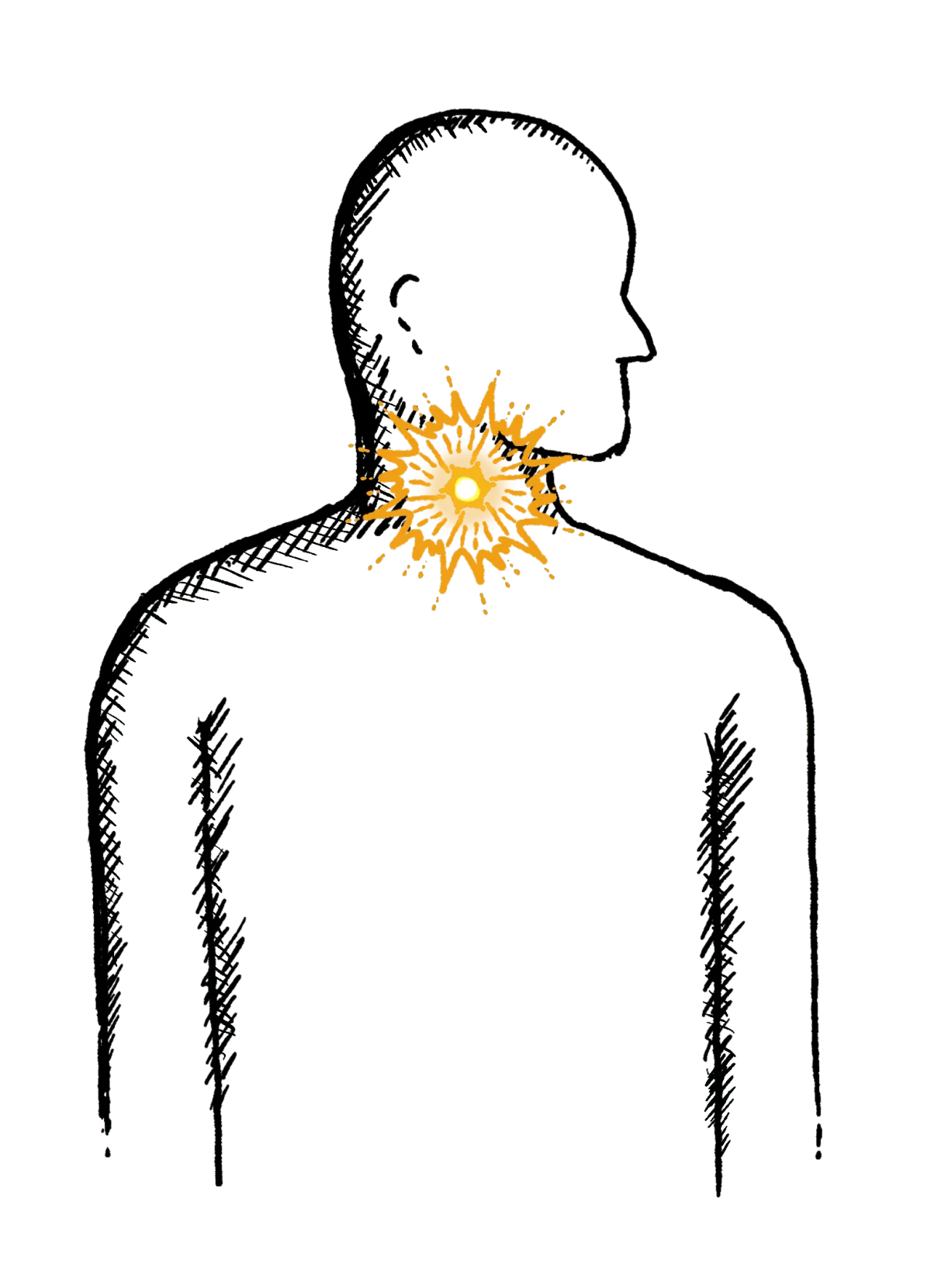
Reflux
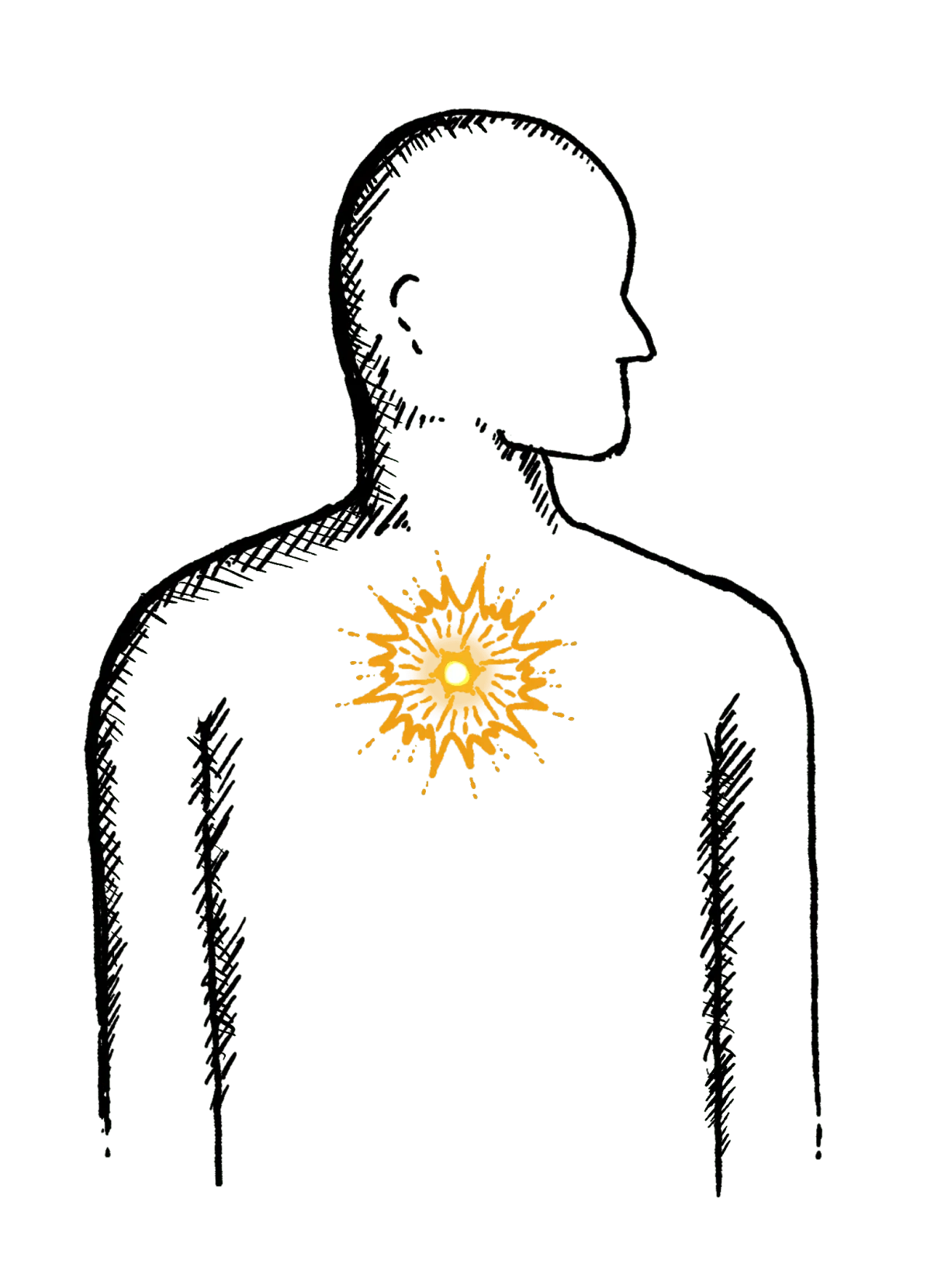
Burning mid-chest, worse when bending or lying down
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
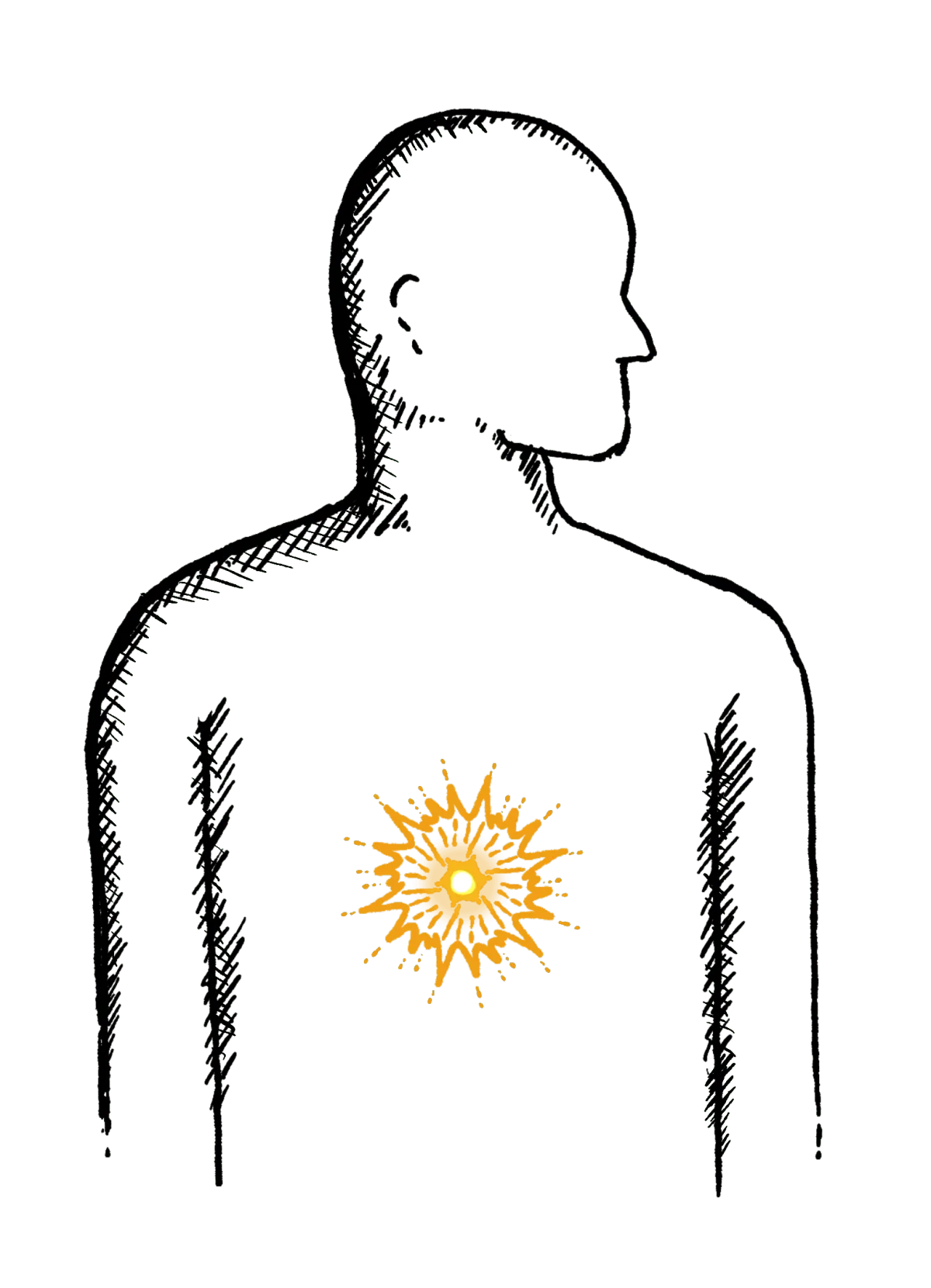
Heartburn
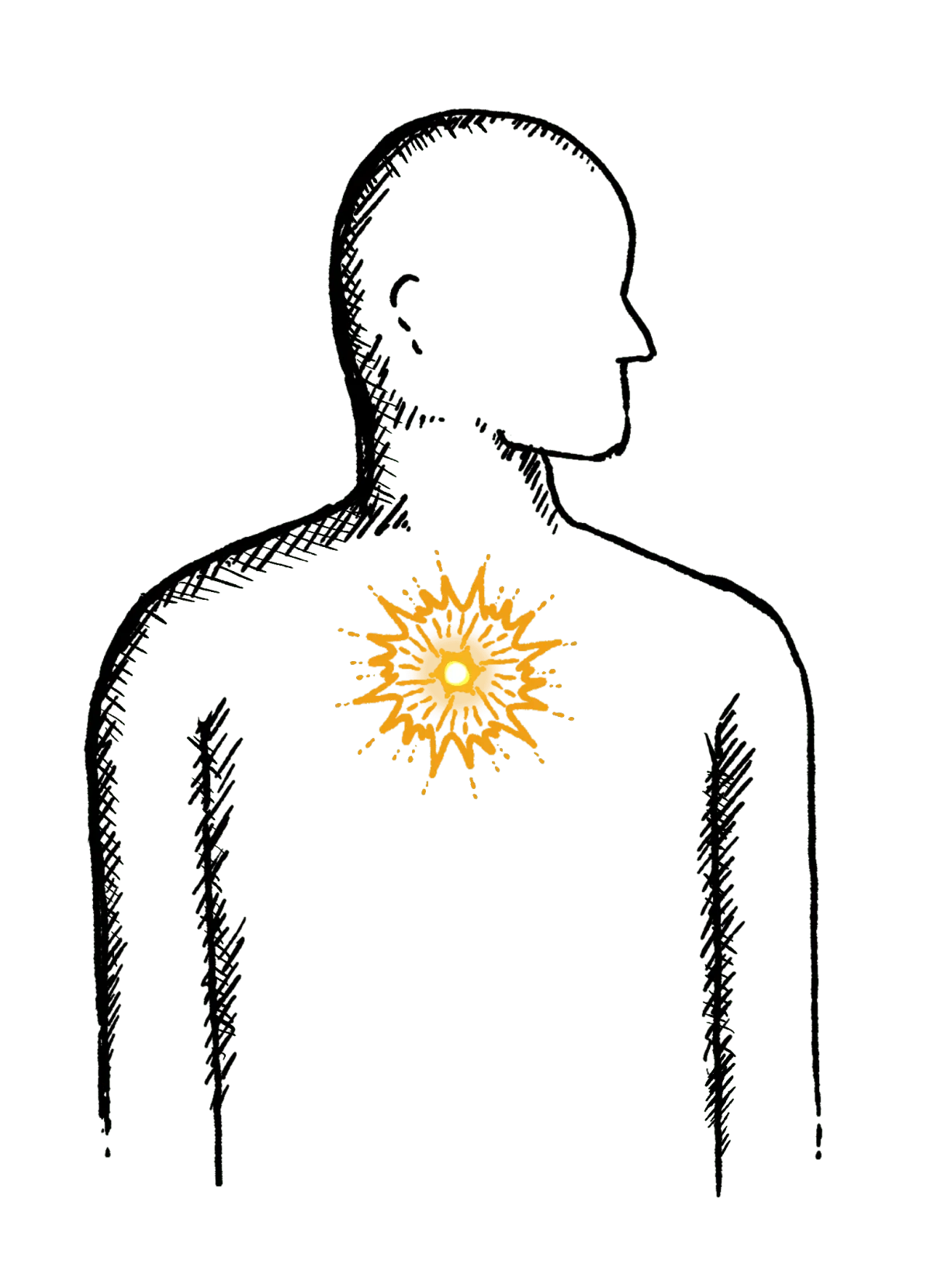
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
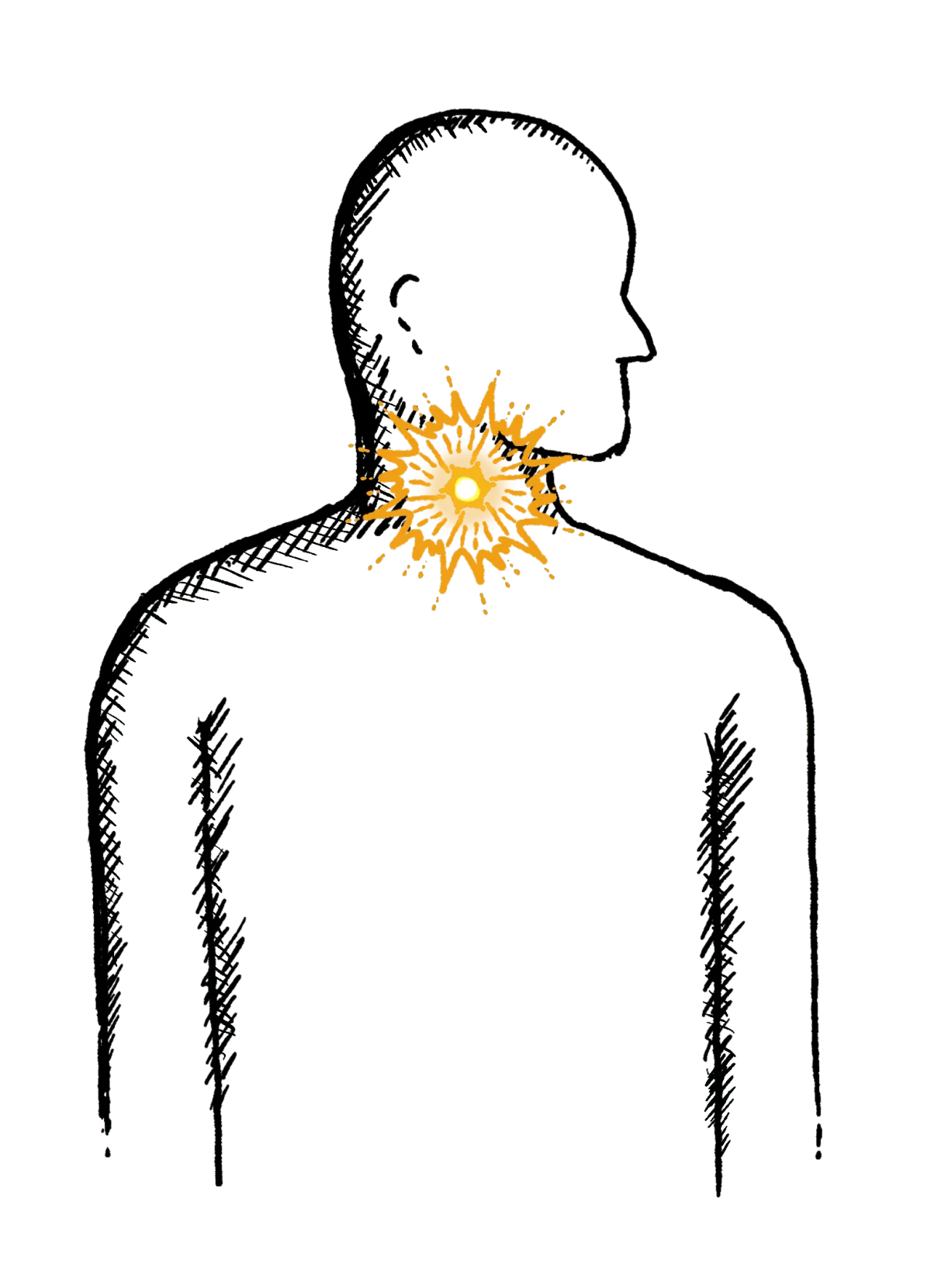
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
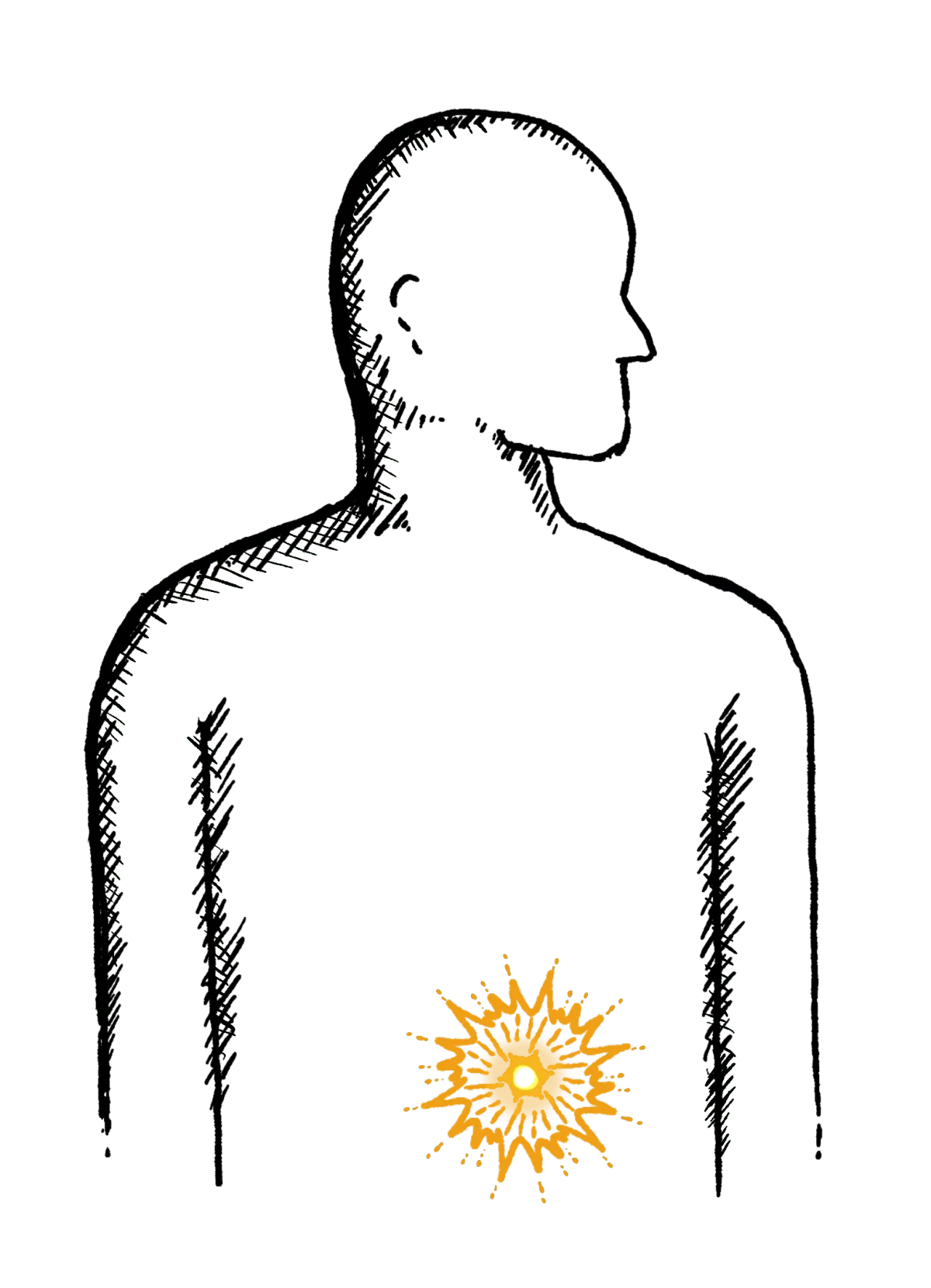
Diarrhoea
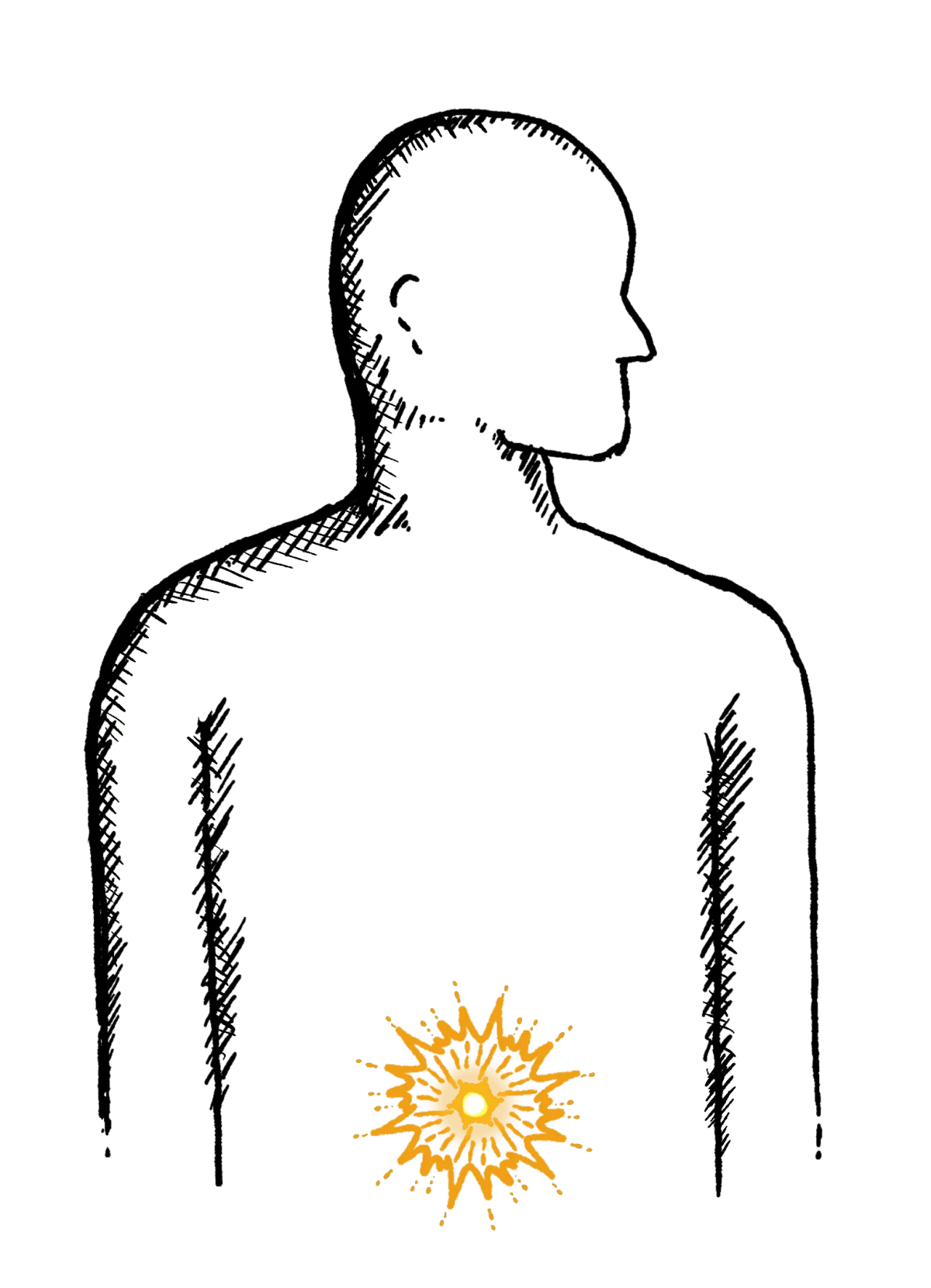
Loose or explosive stools, can’t get to a toilet in time
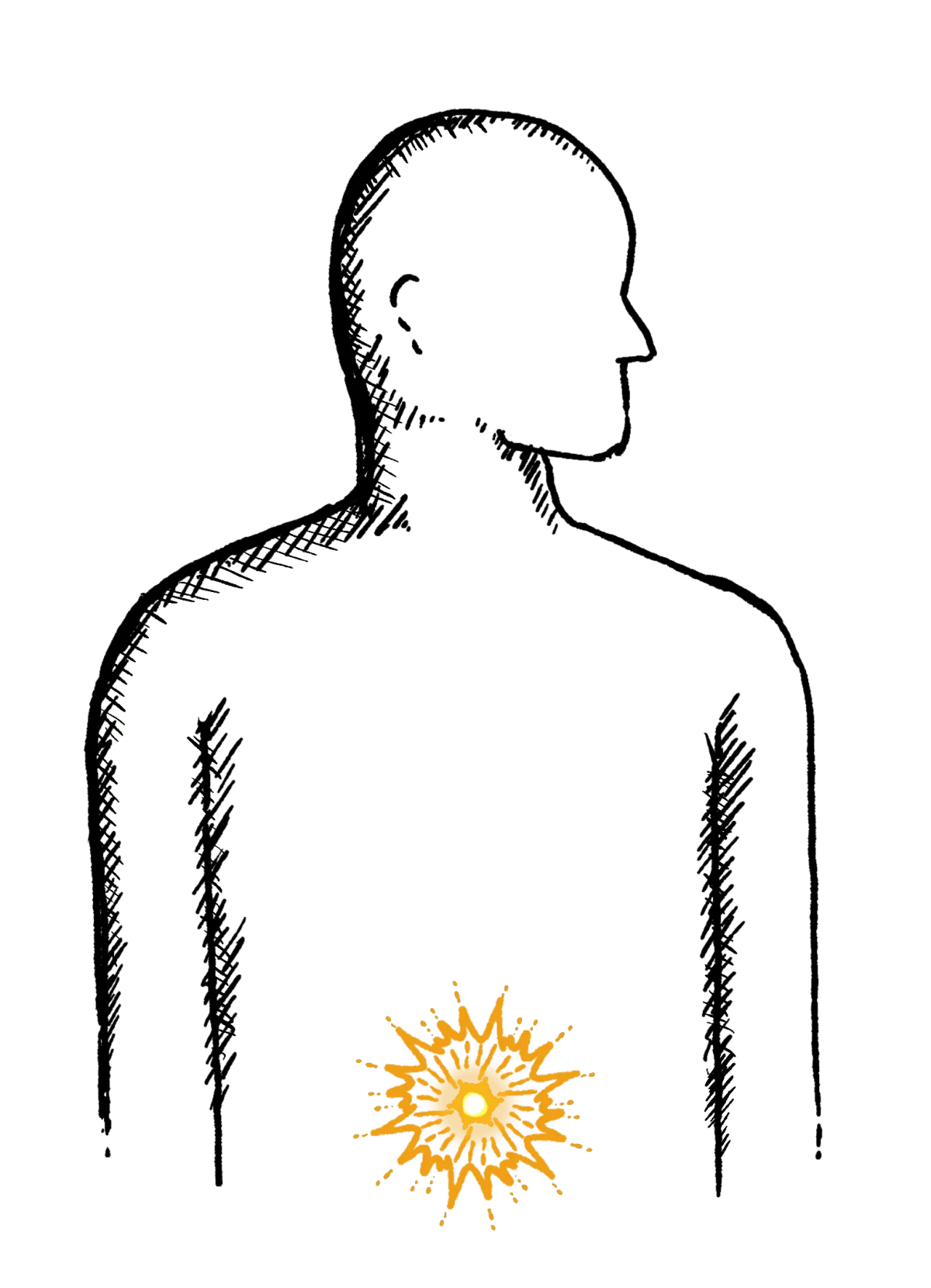
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

