Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

What is Bloating and Distention
What Is Bloating and Distention?
For many patients with irritable bowel syndrome (IBS) and functional gut disorders, one of the most bothersome symptoms is bloating, a sensation of increased abdominal pressure.
Around 50% of patients with bloating also experience distension, an increase in abdominal girth of up to 10cm. Distension can be particularly intrusive, causing many sufferers to avoid wearing certain clothes and not attend social events due to their appearance.
What are the causes of bloating?
The causes of bloating and distension are often multifactorial, meaning individuals may have one or more underlying causes for their symptoms. Although overlapping, research has shown bloating and distension to have differences in their pathophysiology. Hypersensitivity in the abdomen plays a major role in bloating and has a great association with diarrhoea-predominant IBS (IBS-D). Meanwhile, distension is more commonly associated with constipation-predominant IBS (IBS-C), often caused by slow intestinal transit.
Individuals with IBS have been shown to handle gas differently than those without IBS. In one study, IBS patients retained significantly more gas in their abdomen compared to healthy volunteers. This gas retention was linked to increased symptoms of bloating and distension.
Those who struggle with bowel movements, such as people with constipation, also tend to experience more bloating and distension. This is likely due to difficulty clearing gas and stool from the gut, leading to a buildup that causes discomfort.
When the volume in the intestines increases, due to gas or food, the body adjusts through what’s known as the accommodation reflex. In healthy individuals, this reflux involves the internal oblique muscles contracting and the diaphragm relaxing, helping to manage the pressure and prevent visible bloating. However, in people who experience bloating and distension, this response appears to work in reverse. Instead of adjusting normally, their diaphragm contracts and the internal oblique muscles relax, which leads to greater abdominal distension compared to healthy individuals.
Bloating is also seen in patients suffering from small intestinal bacterial overgrowth (SIBO). In healthy individuals, there is a much smaller concentration of bacteria in the small bowel compared to the colon. When gut bacteria over-proliferate the small bowel, they can begin to ferment ingested nutrients before our body absorbs them. The by-products of this fermentation (gases, water and short chain fatty acids) can then lead to symptoms of bloating, diarrhoea and abdominal pain.
Carbohydrate malabsorption can also cause bloating, the most commonly described being lactose malabsorption (hypolactasia). Lactose is the sugar naturally found in dairy products, it is a disaccharide meaning it is made up of two simple sugars (monosaccharides), glucose and galactose. Hypolactasia is a condition where the enzyme lactase becomes depleted in the small bowel. Lactase is required to break down lactose into the two simple sugars before they can be absorbed. If lactase is depleted this process will be impaired leading to fermentation of lactose in the colon, causing bloating amongst other abdominal symptoms. Hypolactasia has a higher prevalence Eastern, African, South American populations compared to European populations.
Even in healthy individuals it is normal for some carbohydrates to enter the colon where they are fermented. These sugars are known as Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs). Where an imbalance of colonic bacteria occurs (dysbiosis), as seen in patients with an irritable bowel, there may be altered fermentation of these carbohydrates in the proximal colon. The production of increased short chain fatty acids as a by-product of colonic fermentation may cause changes to the pH of the gut and altered gut motility. These changes to the environment and motility of the gut in addition to the gases produced as by-product of fermentation may ultimately contribute to bloating and distension.
How can bloating and distension be treated?
Understandably, these symptoms can significantly affect quality of life, so an effective treatment could make a big difference to many IBS patients. Due to the diversity of causes of bloating and distension, treatment will be specific to the underlying causes of bloating. However, a range of methods have been shown to alleviate symptoms for some patients, including dietary modification, medications and physical therapies.
How can SIBO be detected and treated?
A simple breath test may detect if SIBO is responsible for bloating. If positive, specific antibiotic regimes can decrease the bacterial count in the small bowel. By reducing levels of small intestinal bacteria, premature fermentation of ingested foods is reduced, thus alleviating symptoms of bloating.
Can probiotics help to reduce bloating and distension?
If SIBO is not the cause of symptoms other therapies may be considered. As gut microbiota may differ in IBS to those in healthy individuals, alteration of the microbiota with probiotics is a potential target for alleviation of bloating and distension. One study demonstrated that the daily intake of a probiotic yoghurt (Bifidobacterium lactis) alleviated distension in patients with IBS-C through acceleration of intestinal transit. In another study, a combination probiotic (VSL#3) was shown to reduce symptoms of bloating and slowed colonic transit in a proportion of patients.
Despite positive results from several studies, further research into different types of probiotics (species, mixtures, strains), optimum dosage and treatment length are required to better understand the role of probiotics and their effect on bloating and distension. When trialling probiotics, individuals should only use one probiotic at a time allowing them to evaluate the effect of the probiotic on their symptoms more accurately. Individuals should follow manufacturers/healthcare professionals’ dosage instructions and consume for at least 4 weeks.
Can a change in diet help to reduce bloating?
Introduction of a low FODMAP diet may help relieve symptoms by removing these highly fermentable sugars from the diet, thus reducing fermentation. These troublesome sugars are found in foods such as onions, garlic, dairy and some fruits. A low FODMAP diet can be quite restrictive and therefore should be undertaken with the guidance of a registered dietician. The dietician will be able to guide patients on which foods they need to initially restrict, as well as manage the reintroduction of specific foods to make sure there are no shortfalls in the patients’ nutritional intake.
Breath tests can also be carried out to assess whether individuals are malabsorbing specific sugars such as lactose and fructose. By finding out if certain sugars are being malabsorbed it is possible to tailor diets to reduce bloating caused by fermentation of these specific sugars.
What about Faecal Microbiota Transplantation (FMT) and what is it?
There is increasing public and media interest in the topic of FMT and its potential uses. FMT is the process of collecting faeces from a healthy donor, separating the gut bacteria (microbiota) from other faecal matter and transplanting the microbiota into another individual with a disease or disorder relating to the microbiota. The aim of this process is to repopulate the gut of the diseased individual with the microbiota of the healthy individual and thus treating the underlying cause of the disease.
FMT is the most effective treatment for recurrent Clostridium Difficile and research is showing promise in other conditions such as ulcerative colitis. A great deal more research is needed to establish the effectiveness and safety of FMT in other conditions including IBS and this will certainly be a hot topic in coming years.
Are there any medications which can help alleviate bloating and distension?
Antidepressants at a relatively low dose can be used to target bloating. Studies have shown that citalopram can significantly reduce symptoms of bloating through its effect on improving bowel motility and regularity. Other antidepressants such as amitriptyline are also known to improve stool consistency and reduce hypersensitivity of the gut, thus reducing the sensation of bloating.
Other medications have a more specific effect on the bowel. The drug linaclotide increases transit time and reduces visceral hypersensitivity via activation of the enzyme guanylate cyclase C and has been shown to reduce the symptom of bloating and in patients with IBS-C.
The medication ebastine, a antihistamine has been shown to relieve bloating and distension among other IBS symptoms in a recent clinical trial. It works by desensitising the TRPV1 pain receptor, where typically histamine and its metabolites bind, contributing to visceral hypersensitivity.
Are there any physical therapies that can be used to reduce distension?
Biofeedback is a clinical tool used by clinicians and physiotherapists to reduce distension. One study demonstrated the effectiveness of biofeedback by comparing participants with distension to healthy volunteers. Through electrodes attached to the skin, respiratory targeted biofeedback helped to reduce the activity of the diaphragm (by 18% ± 4%) and intercostal muscles (by 19% ± 2%) and increased the activation of the internal oblique muscles (by 52% ± 13%). An average reduction in abdominal girth of 25mm was seen in these patients following this biofeedback technique.
Biofeedback can be utilised in patients with defecatory disorders to improve evacuation techniques, thus reducing bloating and distension. In order to pass stool, it is important to relax the muscles in the back passage. Some individuals inadvertently contract the muscles in the back passage, which acts as a barrier to passing stools, known as dyssynergia. Pelvic floor targeted biofeedback conducted by a trained physiologist or physiotherapist can help individuals to visualise their bad toileting technique and correct it.
Although there is a large range of treatment options targeting the various causes of bloating and distention, they will not all work for everyone. It is important to identify the underlying mechanisms and contributing factors behind the symptoms on a case-by-case basis to select the most effective treatment for each patient.
Think you could benefit from some biofeedback therapy to target your troublesome GI symptoms? Contact us today to see how we can help you.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
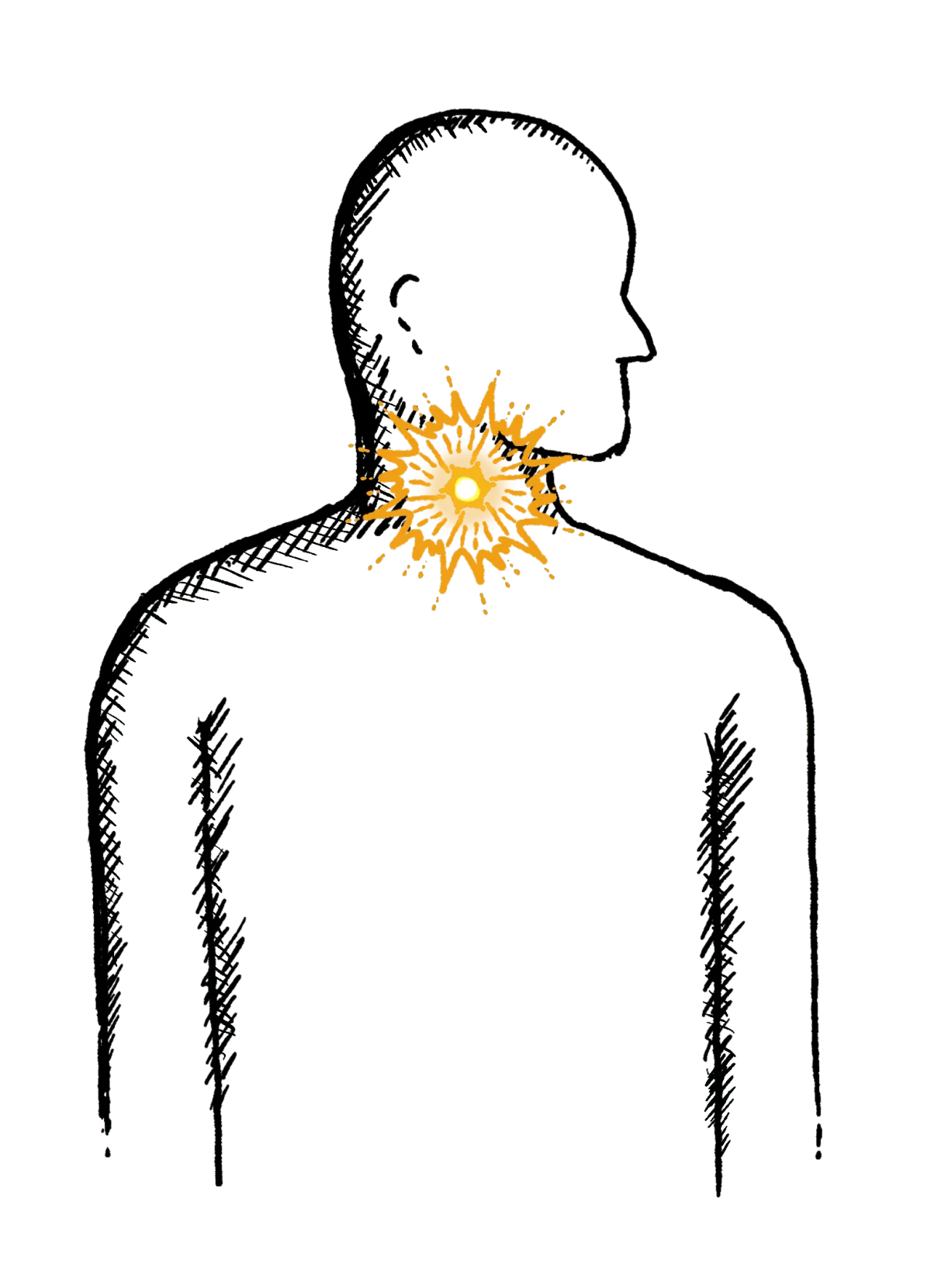
Reflux
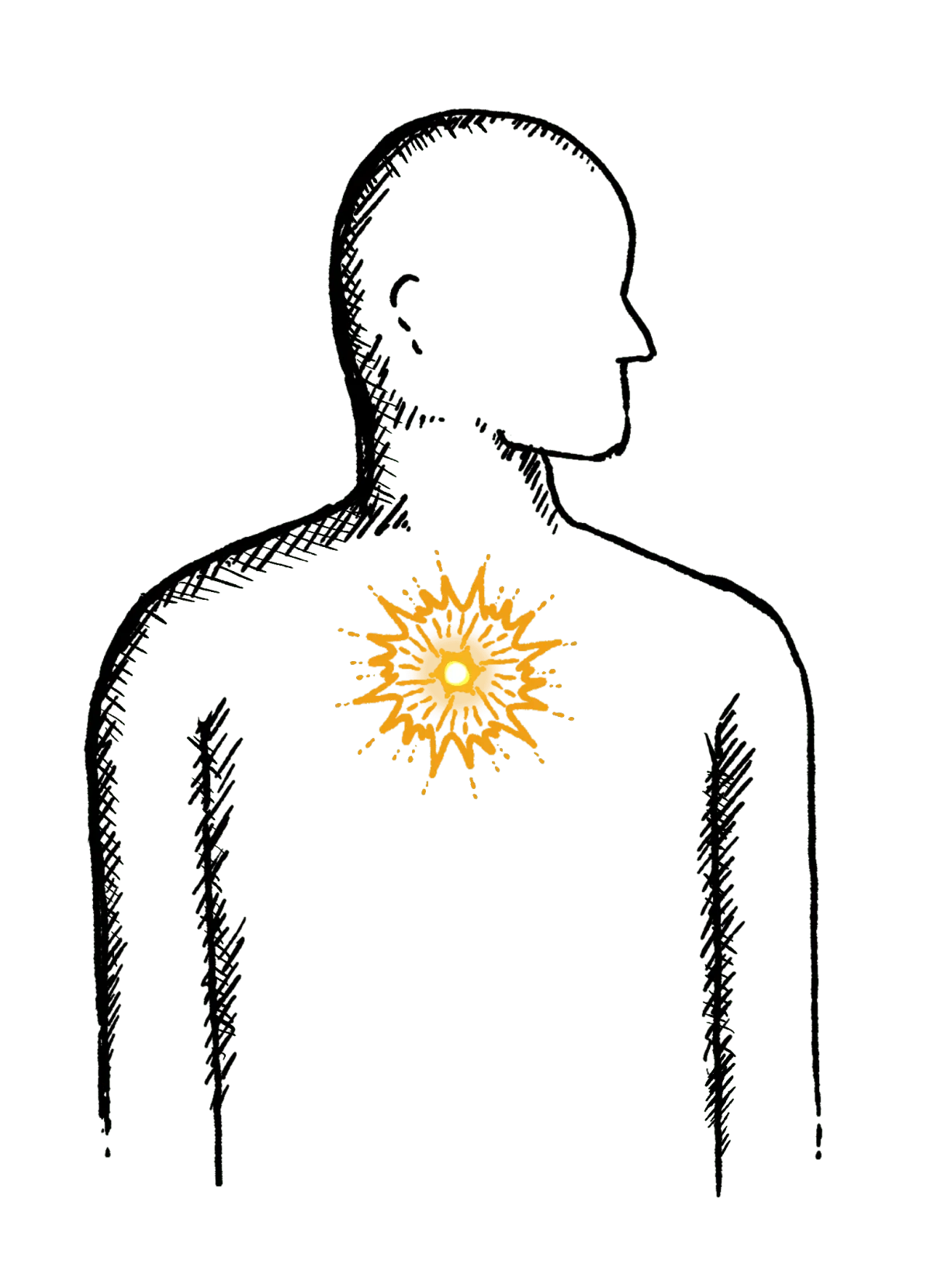
Burning mid-chest, worse when bending or lying down
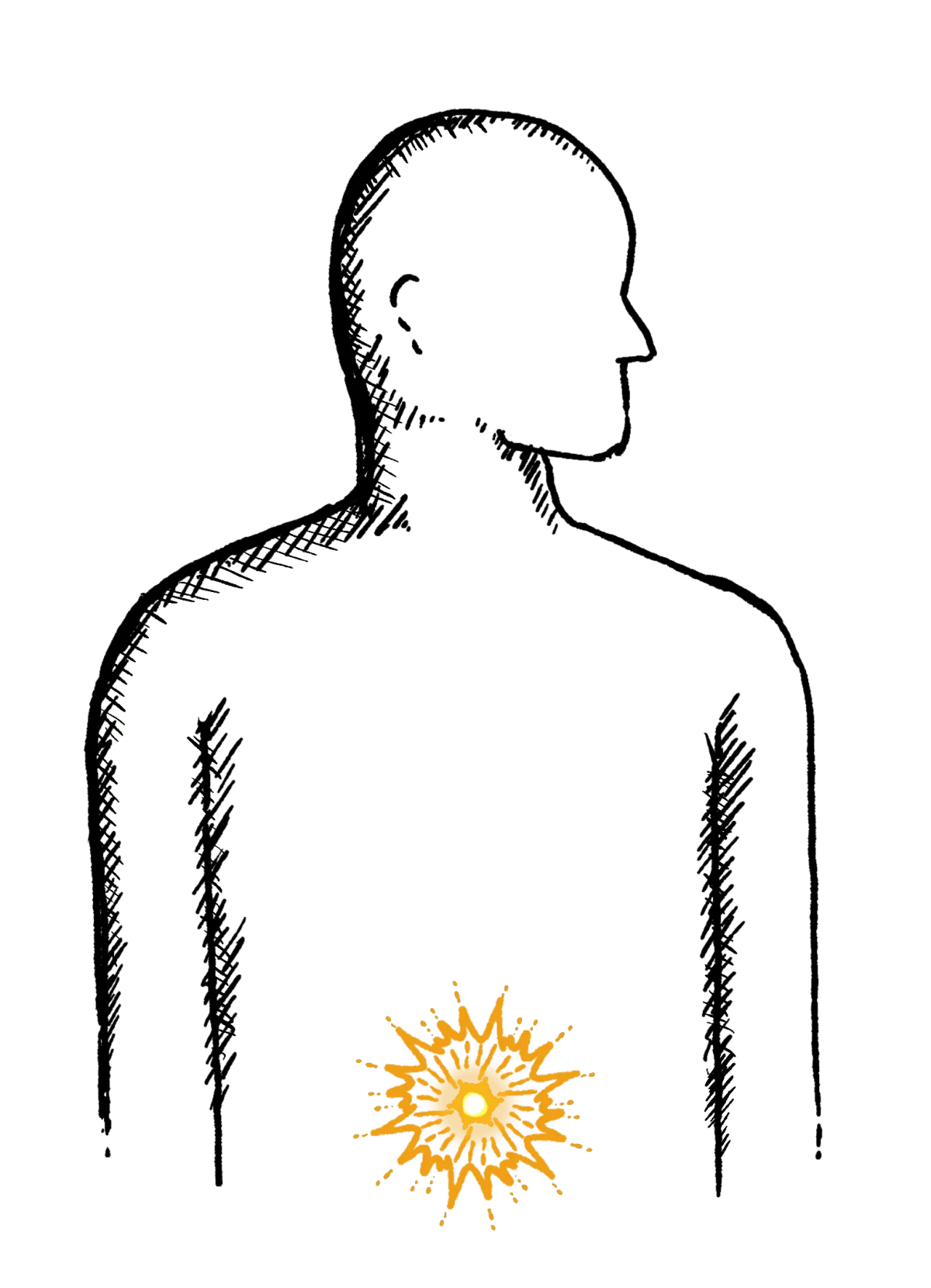
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
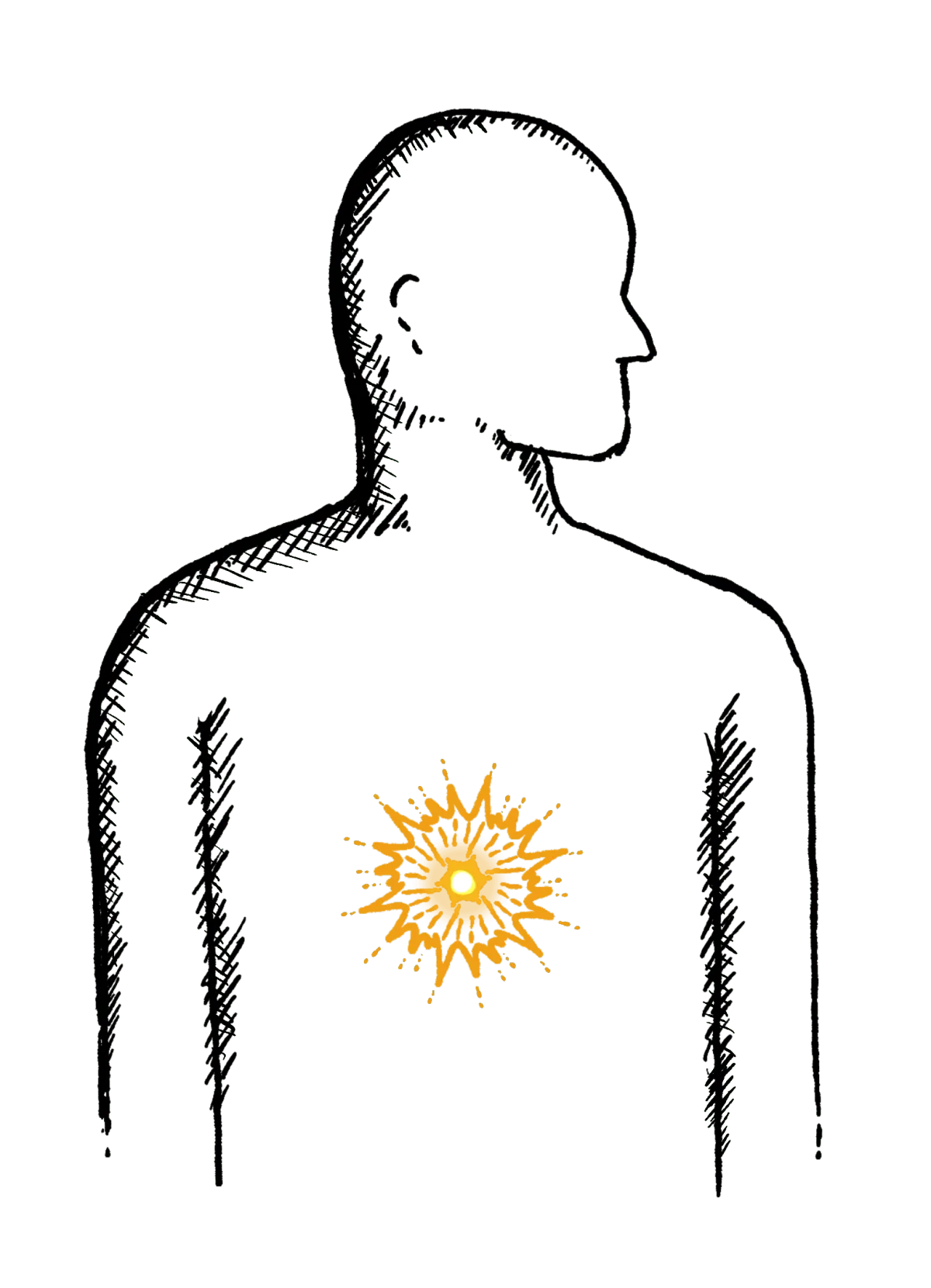
Heartburn
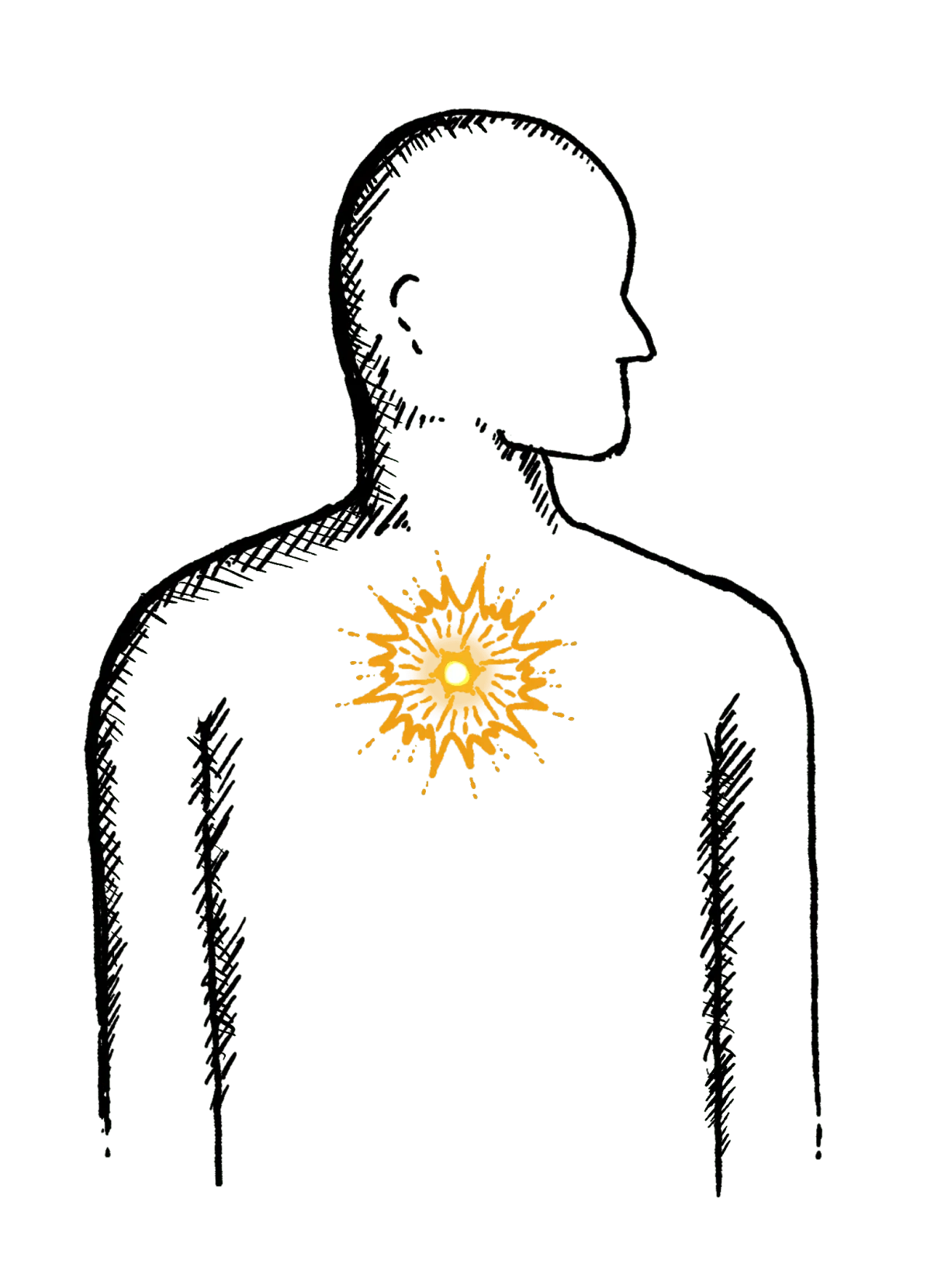
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
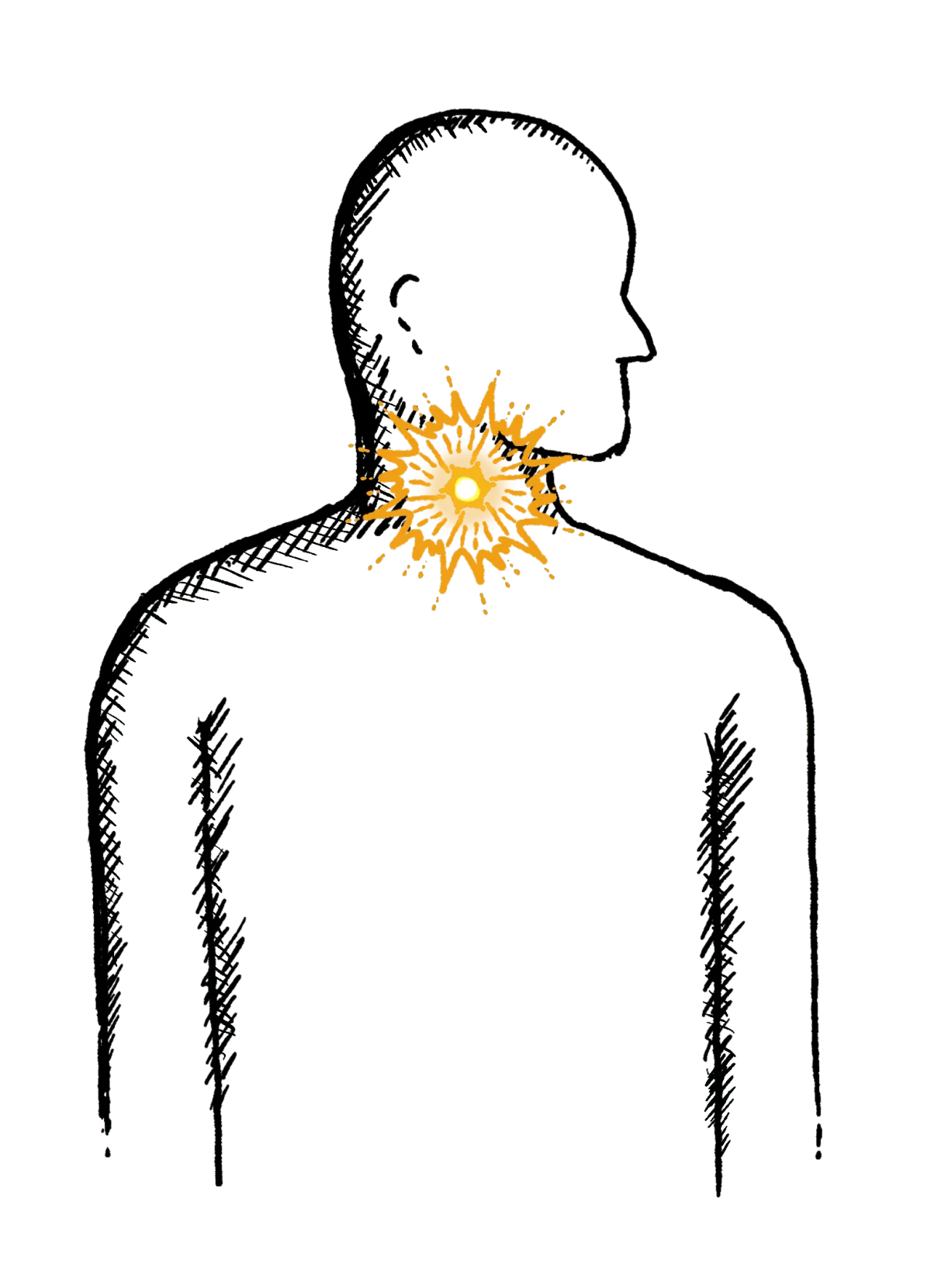
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Diarrhoea
Loose or explosive stools, can’t get to a toilet in time
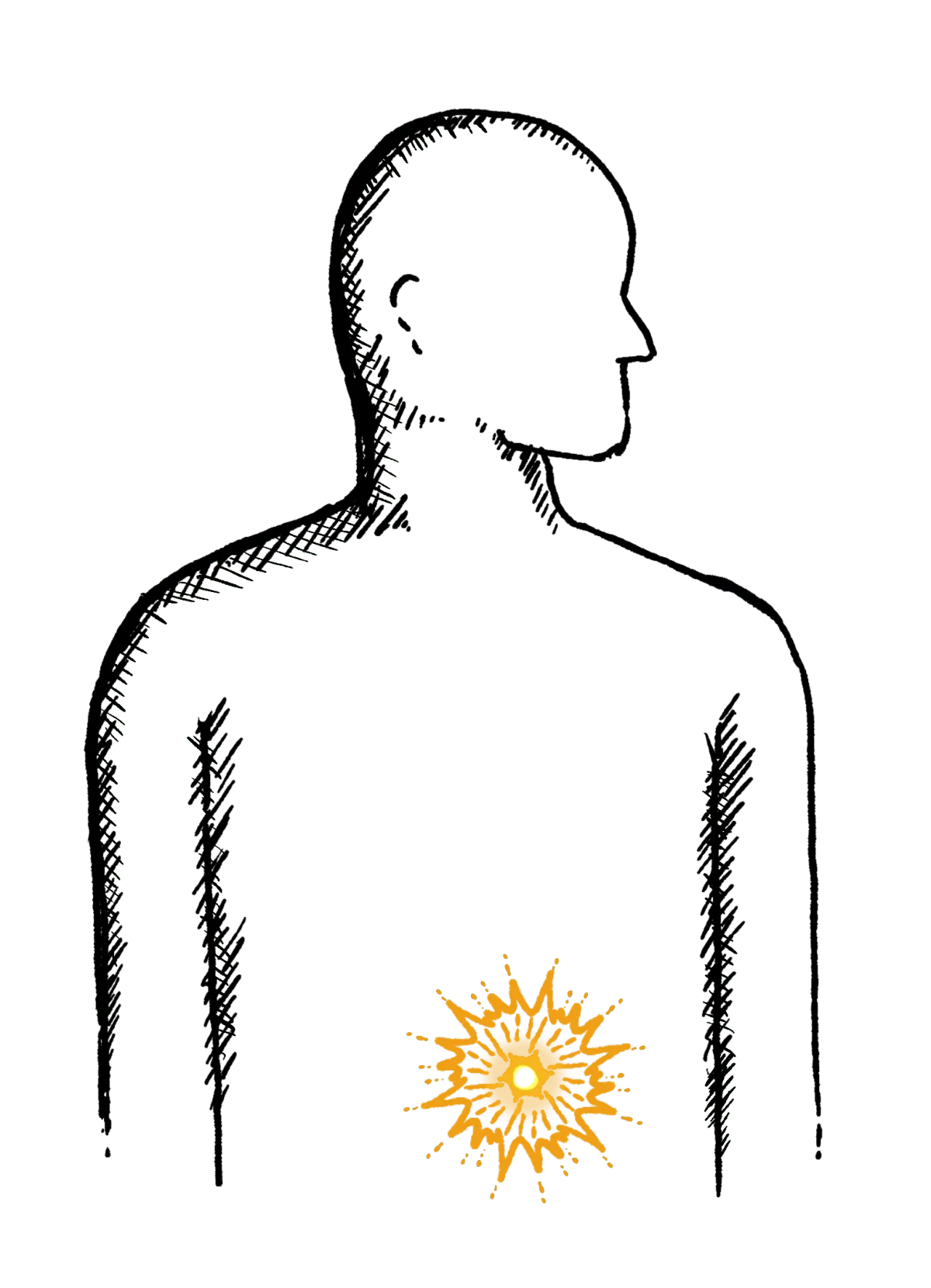
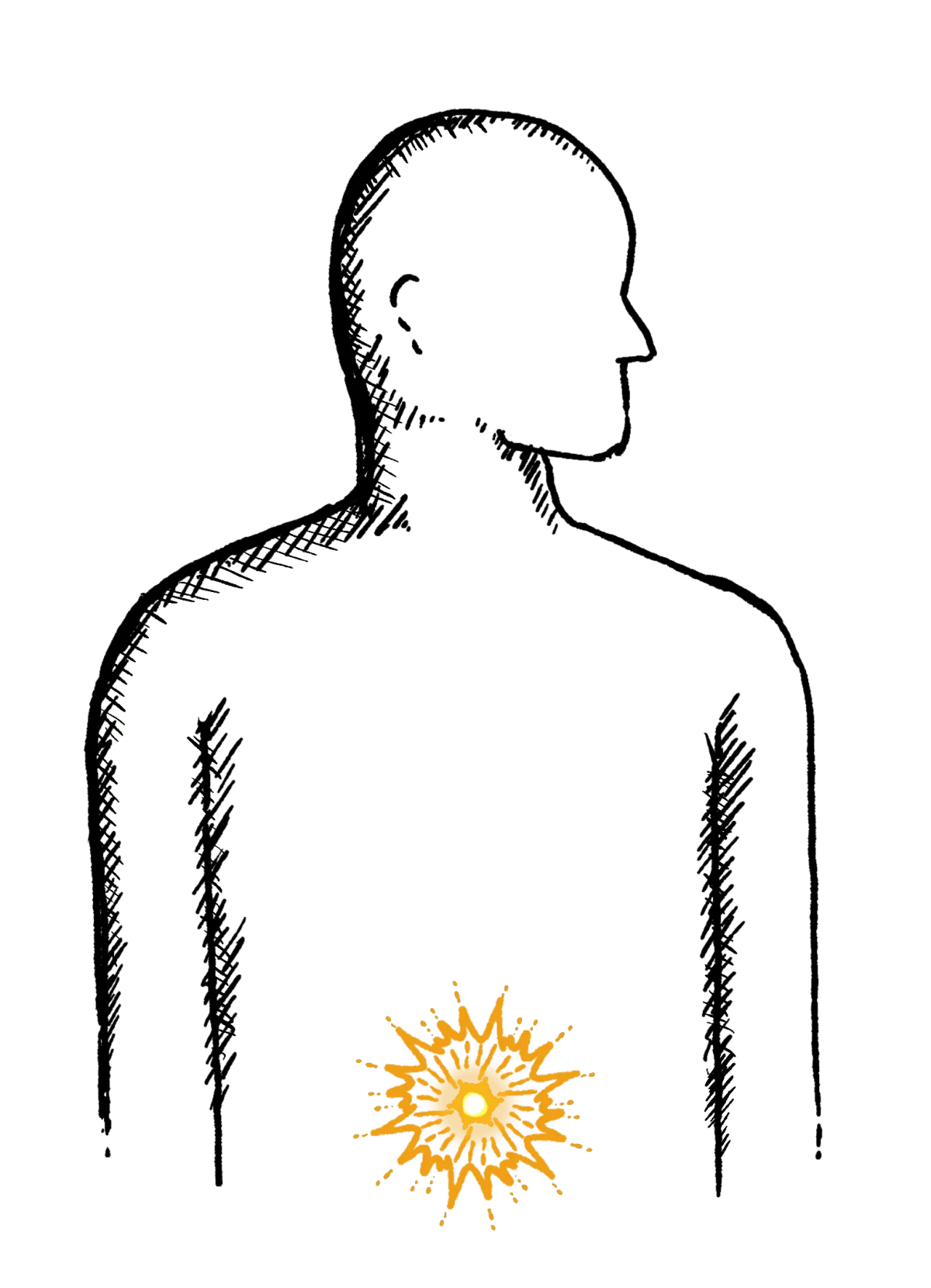
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

