Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating
What Is Hiatal Hernia: Causes, Symptoms, & Treatment
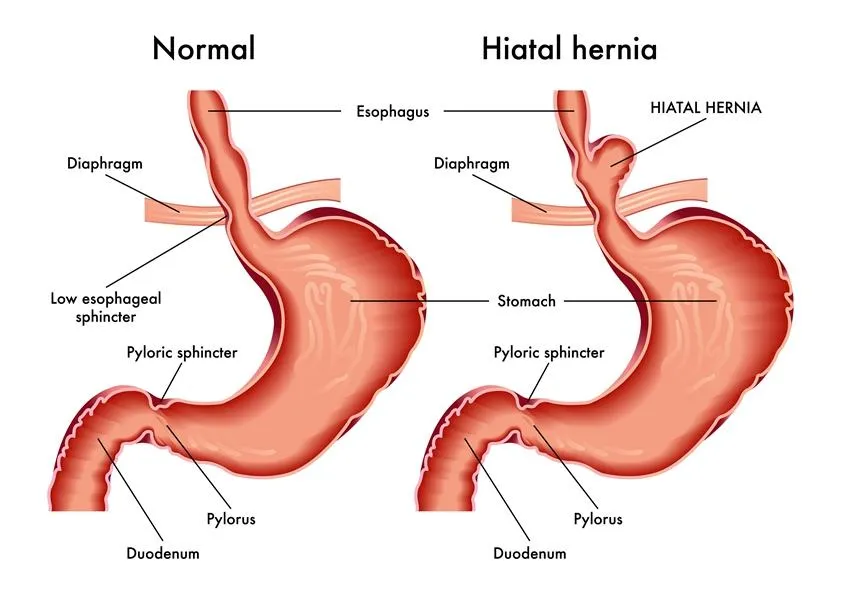
A hiatal hernia (or hiatus hernia) occurs when the upper part of the stomach pushes through the diaphragm and enters the chest. The diaphragm is a muscular layer that separates the chest from the abdomen. People with a hiatal hernia can experience heartburn, acid reflux, and chest pain.
The condition might sound severe but it’s actually pretty common, especially as you get older. Most people only experience mild symptoms of acid reflux (or no symptoms at all). However, in extreme cases, surgery or medication might be needed to manage the condition.
What Is a Hiatal Hernia?
A hiatal hernia is the presence of the stomach above the diaphragm. Your diaphragm is a muscular barrier separating the abdominal cavity from the chest cavity and helps you breathe. If there is weakness in the diaphragm, increased abdominal pressure can push the stomach upwards.
It’s also known as a hiatus hernia or esophageal hiatus. The condition develops slowly over many years.
Usually, food passes from the mouth into the throat, down the esophagus, to the stomach. The stomach and esophagus are separated by the lower esophageal sphincter (LES). With a hiatus hernia, the LES is weakened, increasing the risk of acid reflux and gastroesophageal reflux disease (GERD).
Types of Hiatal Hernias
There are two main types of hiatal hernias: sliding hiatal hernias and paraesophageal hiatal hernias. These are classified into four categories:
Type 1, or a sliding hiatal hernia, accounts for 95% of all cases. The stomach and esophagus slide up through the widened hiatus and back down again.
Type 2 is the first of three paraoesophageal hiatal hernias. Meaning “beside the esophagus,” this condition involves the stomach pushing up alongside the esophagus, forming a bulge. Also called a rolling hiatal hernia.
Type 3 is a combination of type 1 and 2. Part of the stomach bulges alongside the esophagus, while another part slides in and out.
Type 4 is relatively rare. Here, the hiatus is wide enough for other organs to enter the chest cavity, such as your intestines, pancreas, or spleen.
Symptoms of a Hiatal Hernia
Most people with a hiatal hernia (especially type 1) will not experience any symptoms. If symptoms occur, they’re often linked to GERD and acid reflux. These symptoms include:
Heartburn or acid reflux
Regurgitation of food or sour liquid
Difficulty swallowing
Chest or upper abdominal pain
Feeling full quickly after eating
Shortness of breath (in larger hernias)
If left untreated, severe acid reflux (caused by a hiatal hernia) can cause changes in the esophageal lining. If you notice any vomiting blood, coffee-ground vomit, or passing black stool, seek immediate medical attention – it is a potential sign of cancer.
What Causes a Hiatal Hernia?
The term “hernia” describes any internal part of the body pushing through a weak spot in the surrounding muscle or tissue wall. Usually, a hiatal hernia refers to an abdominal hernia, where the intestines protrude out of the abdomen.
If a weak spot develops in the diaphragm, the stomach can begin to push through. This is a gradual process, with the hiatus incrementally increasing due to years of stress and strain. Anything that raises the abdominal pressure will wear on your diaphragm over time.
Common causes include:
Persistent coughing or sneezing
Long-term constipation and straining
Obesity (BMI over 30)
Frequent vomiting
Heavy lifting or intense exercise
Pregnancy and childbirth
More rarely, a hiatal hernia can occur as a result of a specific injury, surgery, or a birth defect. This creates the initial weakness, which worsens over time. Often, these conditions present with more severe hiatal hernias as they’ve had more time to develop.
Diagnosing a Hiatal Hernia
The simplest way to diagnose a hiatal hernia is to visualize what’s going on inside. Your doctor may recommend these tests:
Barium swallow—a person drinks a cup of barium, which allows the esophagus and stomach to be seen on an X-ray. It can provide a clear image of where the stomach is within the chest or abdomen.
Endoscopy – a thin, flexible tube with a camera on the end is passed down the esophagus and into the stomach. It can be seen directly if the stomach is pushing on the diaphragm, along with any obstructions or strangulation.
Esophageal manometry – a thin, flexible tube with pressure sensors is passed through the nose and down into the stomach. The measured pressures can detect the presence of a hiatus hernia as well as accurately measure its size. It can also help distinguish a hiatal hernia from other esophageal motility disorders, such as Achalasia.
Treatment of Hiatal Hernias
Most people with a hiatal hernia won’t require any treatment. It’s a normal part of aging. However, if the hiatal hernia is causing recurrent acid reflux (or GERD), it’s advisable to seek treatment.
Your doctor may recommend:
Antacids – to neutralize the acid during an attack.
Proton pump inhibitors (PPIs) – to prevent stomach acid production.
H2-receptor blockers – to lower stomach acid production.
Lifestyle changes may also be necessary, including cutting out foods that cause reflux symptoms.
Struggling with persistent regurgitation or acid reflux symptoms? If you’re dealing with a hiatal hernia, we can help. Learn more about our testing options and take the first step towards a clear diagnosis and effective treatment plan.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
Reflux
Burning mid-chest, worse when bending or lying down
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
Heartburn
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Diarrhoea
Loose or explosive stools, can’t get to a toilet in time
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

