Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

What Is Zenker’s Diverticulum? Symptoms, Causes & Treatment
Zenker’s diverticulum is a pouch that forms in the back of your throat. When you eat, food can become stuck in the pouch, leading to regurgitation and bad breath. The condition occurs when the muscle between your esophagus and throat doesn’t relax, preventing food from moving down to the stomach.
Food regurgitation is an issue with many conditions, including acid reflux. Zenker’s diverticulum is one potential cause that’s often considered. It also presents with difficulty swallowing or a sensation of something stuck in the throat.
But what is Zenker’s diverticulum? Why does it occur? And what is the treatment? Join The Functional Gut Clinic as we answer your questions.
What is Zenker’s Diverticulum?
The term diverticulum refers to a pouch or pocket-like structure. Most often, it occurs in the colon when the inner lining of the intestine protrudes outwards.
Zenker’s diverticulum is a special case. It forms at the lowest part of the throat (pharynx), where it merges with the esophagus. The pocket is typically located on the back wall of the pharynx and can enlarge significantly over time.
The condition is relatively rare and is most common among older people, especially those aged 70-years and older. It affects less than 0.01% of the population. Nobody knows the exact causes, but it seems to be connected to an increase pressure in the esophagus.
Zenker’s Diverticulum Symptoms
The most common symptom of Zenker’s diverticulum is difficulty swallowing. It is experienced in 80-90% of cases. Food easily becomes lodged in the pocket, which can close up the throat and esophagus, giving that sensation of not being able to swallow.
But that’s not the only symptom. Other symptoms include:
Regurgitation of undigested food – often hours after eating
Chronic cough – particularly after eating
Halitosis (bad breath) – due to trapped food in the pouch
Gurgling sounds in the neck - during swallowing
Aspiration – food or liquids entering the airway
Hoarseness or voice changes
Weight loss – in more advanced or chronic cases
Neck mass – sometimes palpable and may increase in size when coughing or straining
Sensation of a lump in the throat (globus sensation)
Causes of Zenker’s Diverticulum
Swallowing might feel like second nature. However, it’s an extremely complicated process involving more than thirty muscles. As you swallow, several muscles work in sync to move the food or liquid out of the mouth, down the throat, and into the esophagus.
Zenker’s diverticulum occurs just above the cricopharyngeal (CP) muscle – where your esophagus and pharynx join. In some people, increased pressure in the esophagus causes the CP muscle to malfunction.
A pouch begins to form as the pressure stretches the lining, gradually worsening over time. Often, there is an initial tear in the esophagus, which allows the lining to protrude outward. Gastroesophageal reflux disease (GERD) is linked to the condition, as it can degrade the esophageal lining and increase pressure in the region.
Zenker’s Diverticulum Diagnosis
Zenker’s diverticulum is often mistaken for other conditions, including GERD or esophageal achalasia. It's also important to differentiate its symptoms from those of gastroparesis, where delayed stomach emptying can lead to nausea, vomiting, and early satiety. People may not realize what the issue is until they develop aspiration pneumonia (a severe bacterial infection due to inhaling regurgitated food).
To make a diagnosis of Zenker’s Diverticulum, your doctor will initially take your history and perform a physical examination. To help diagnose Zenker’s diverticulum, your healthcare provider may recommend the following tests:
Esophageal manometry – Measures the pressure and coordination of muscle contractions in your esophagus to assess how well it’s functioning.
Barium swallow (esophagram) – A type of X-ray where you swallow a barium solution which can show the shape and movement of your esophagus in real time.
Upper endoscopy (esophagogastroduodenoscopy) – Involves inserting a thin, flexible tube with a camera down your throat to examine the inside of your esophagus and rule out other conditions.
These tests can help differentiate between GERD, achalasia, Zenker’s diverticulum, and other potential causes.
Treatment Options
Zenker’s diverticulum isn’t dangerous in most cases. Mild cases are usually treated with a “wait and see” approach. Your doctor will not want to operate or treat the condition if it isn’t affecting your quality of life.
That being said, you might be advised to change your eating habits. Chewing more slowly, taking smaller bites, and drinking between bites can reduce the risk of food getting stuck in the pouch and aspiration pneumonia.
If the condition continues to worsen, more intensive options can be considered.
Surgical Treatment
Moderate to severe cases of Zenker’s diverticulum typically require surgical intervention. There are two primary options:
Endoscopy. In this procedure, the surgeon threads a thin, tube-like instrument with a camera down your throat. It can find the diverticulum and make small incisions to repair the damage or remove the pouch.
Open Surgery. More severe cases, where the pouch is large, requires an incision directly into the neck. Known as a diverticulectomy. This involves separating the diverticulum from your esophageal wall which is then either removed or inverted. The procedure has a high success rate.
Concerned About Regurgitation or Swallowing Issues?
If you're experiencing food regurgitation, persistent coughing after meals, or difficulty swallowing, Zenker’s diverticulum could be one of several possible causes. Understanding your symptoms is the first step toward effective treatment.
Learn more about regurgitation symptoms and when to seek help.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
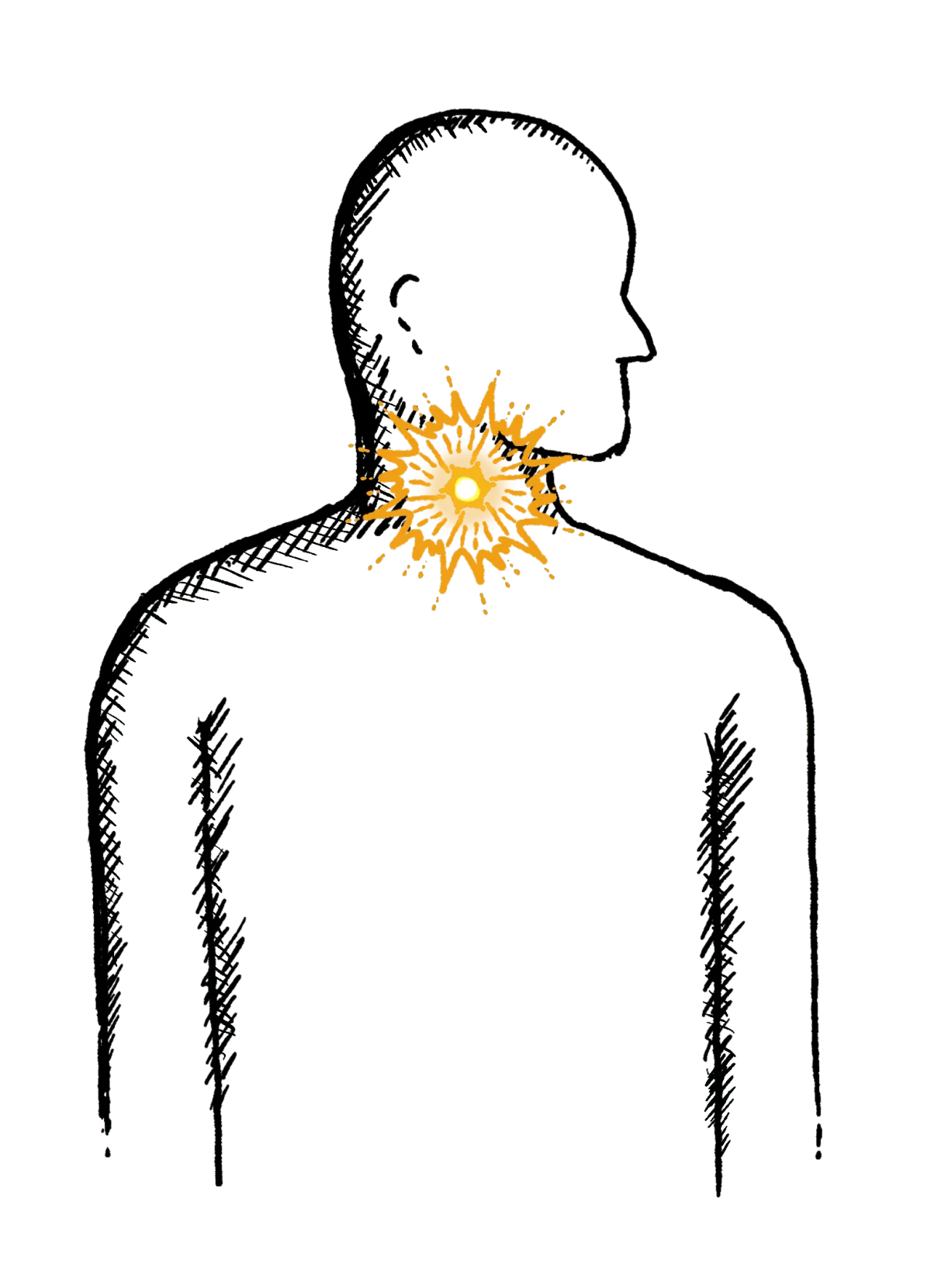
Reflux
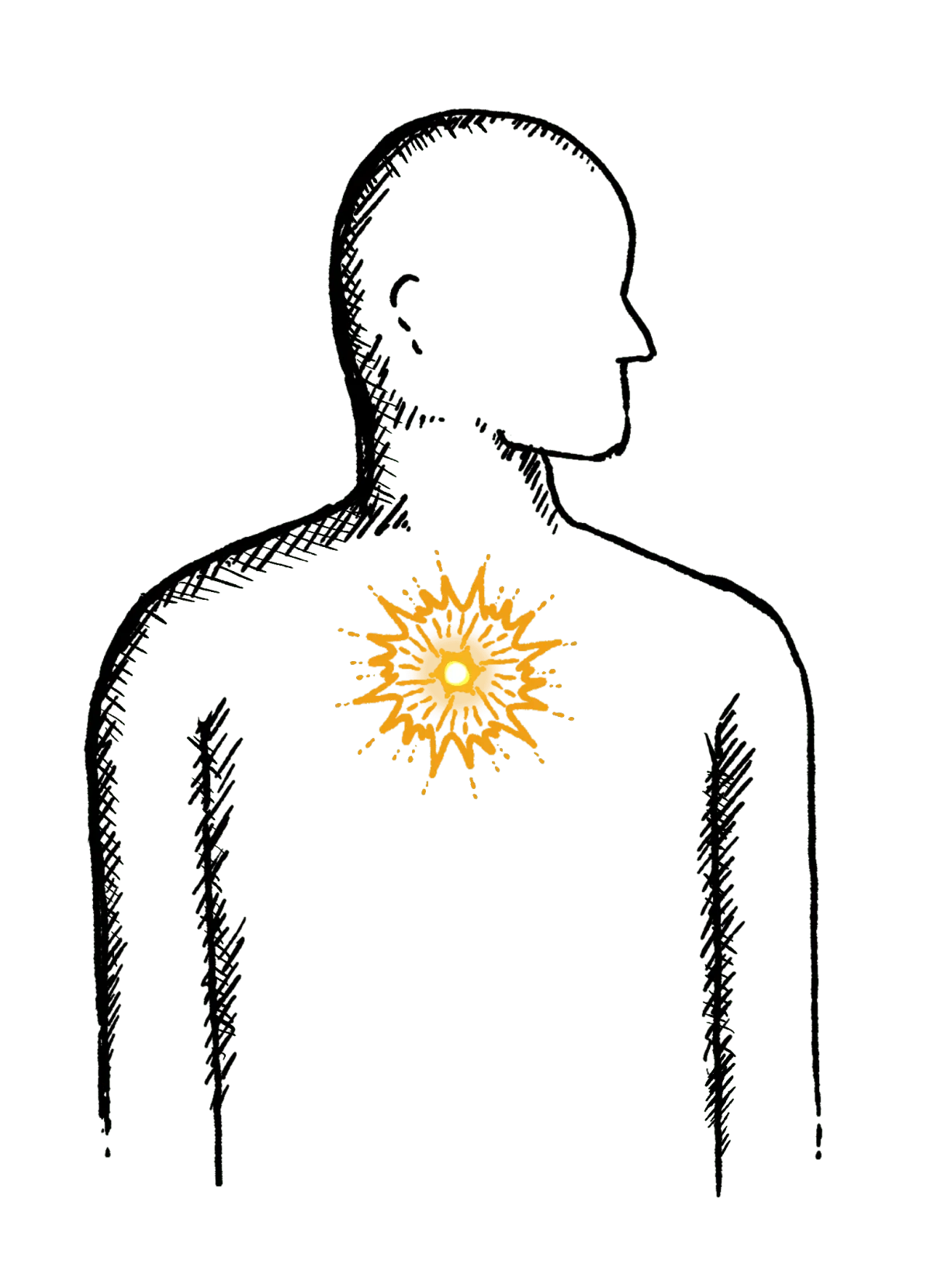
Burning mid-chest, worse when bending or lying down
Constipation
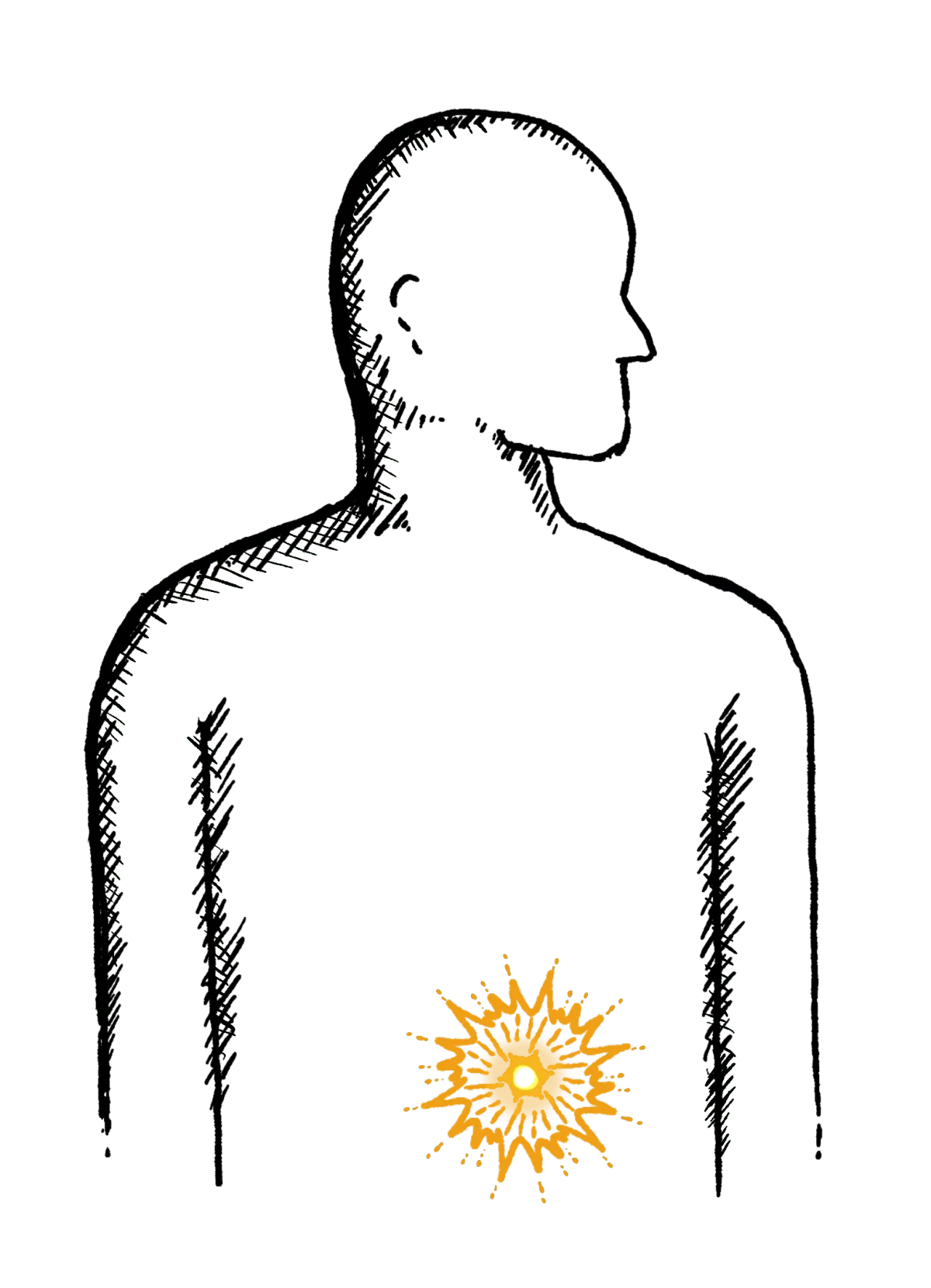
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
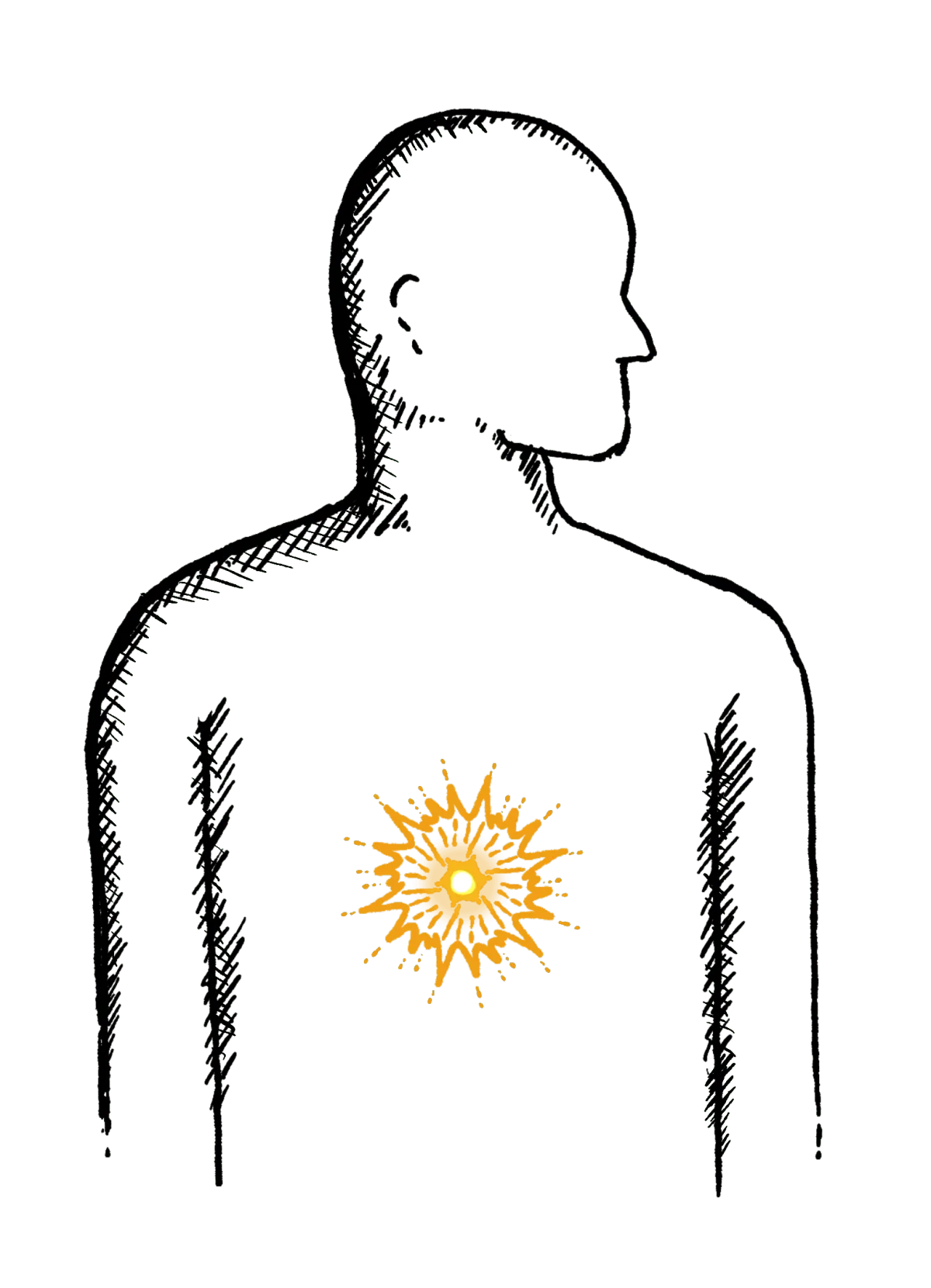
Heartburn
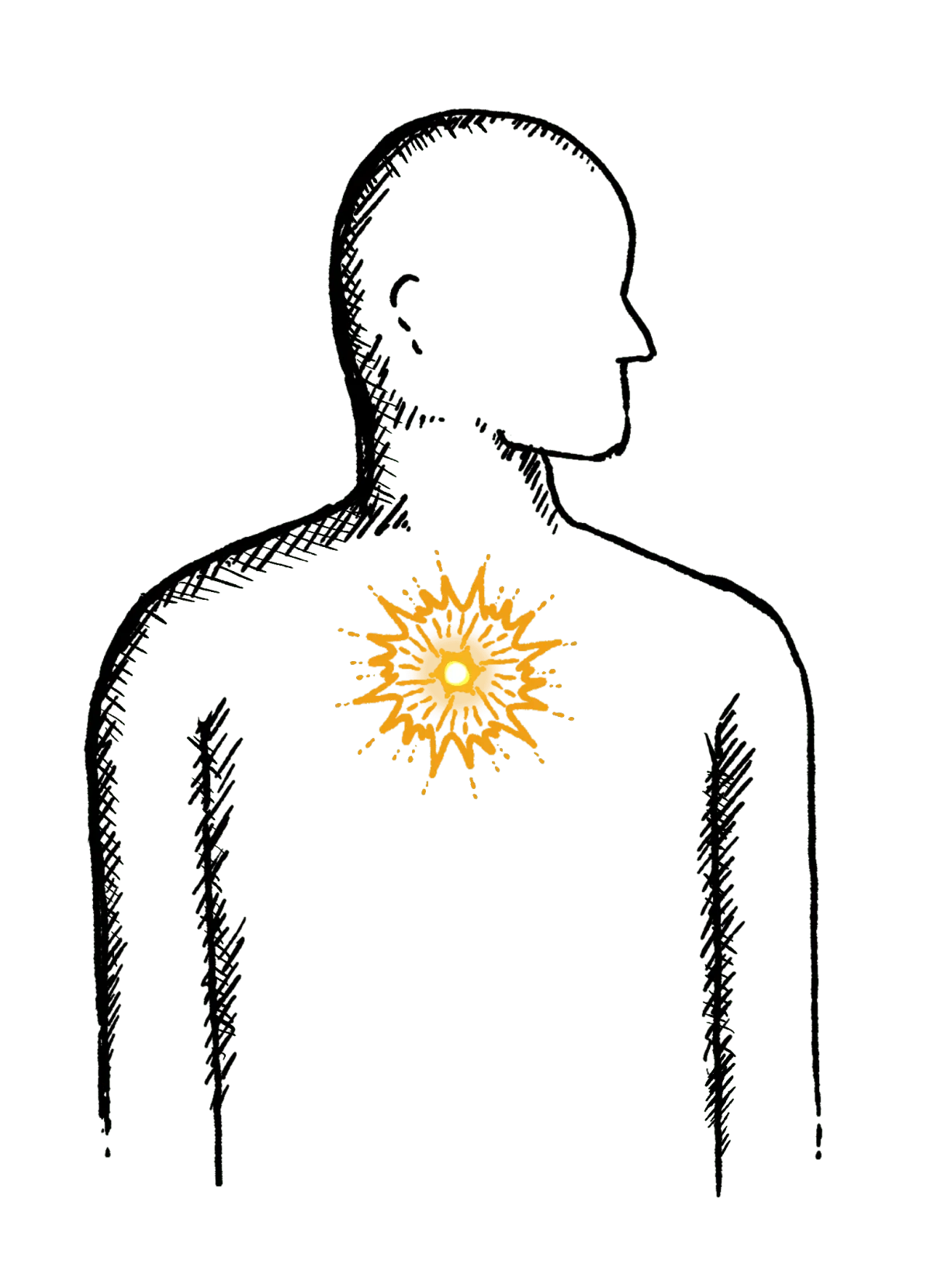
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
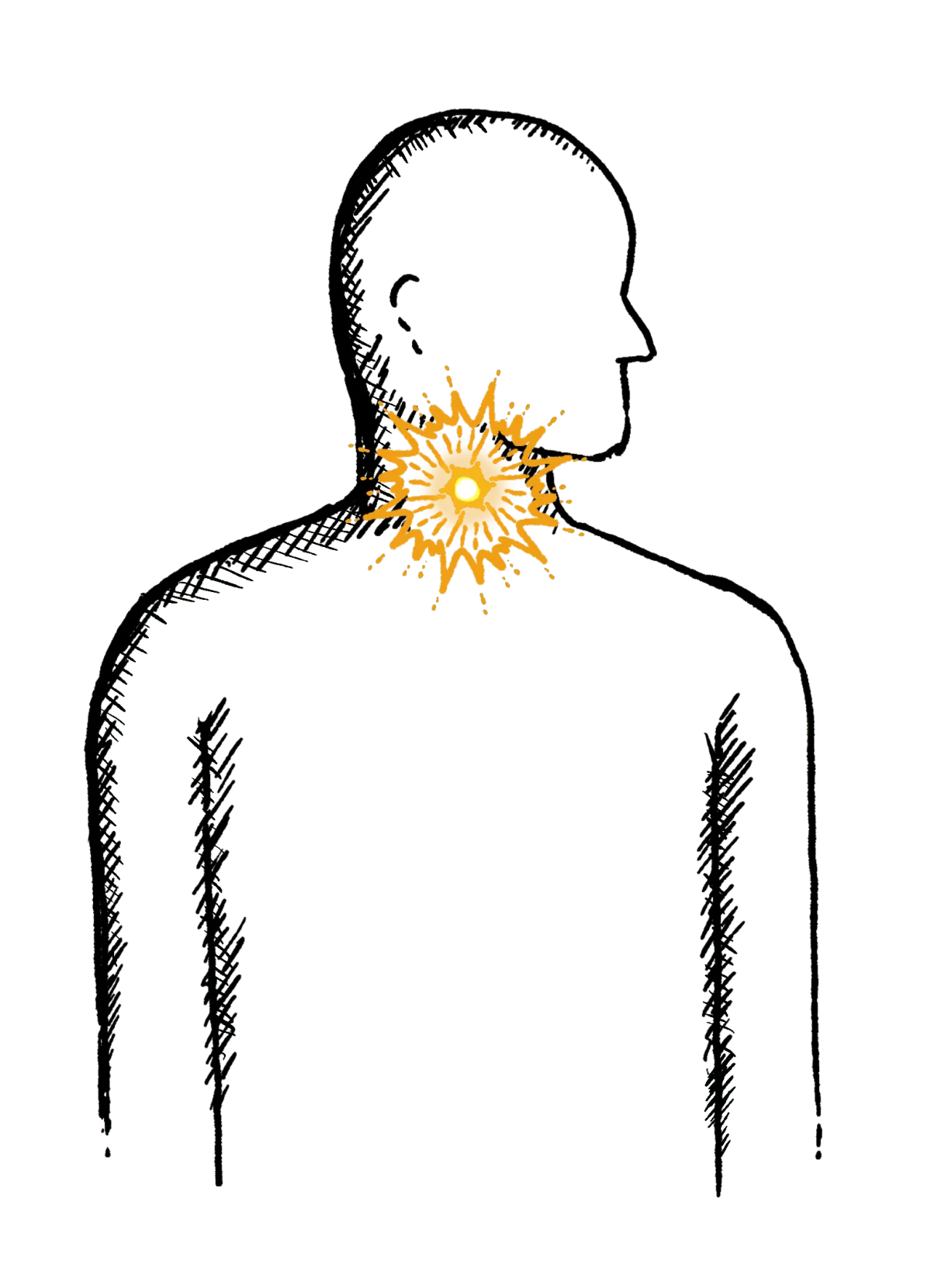
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Diarrhoea
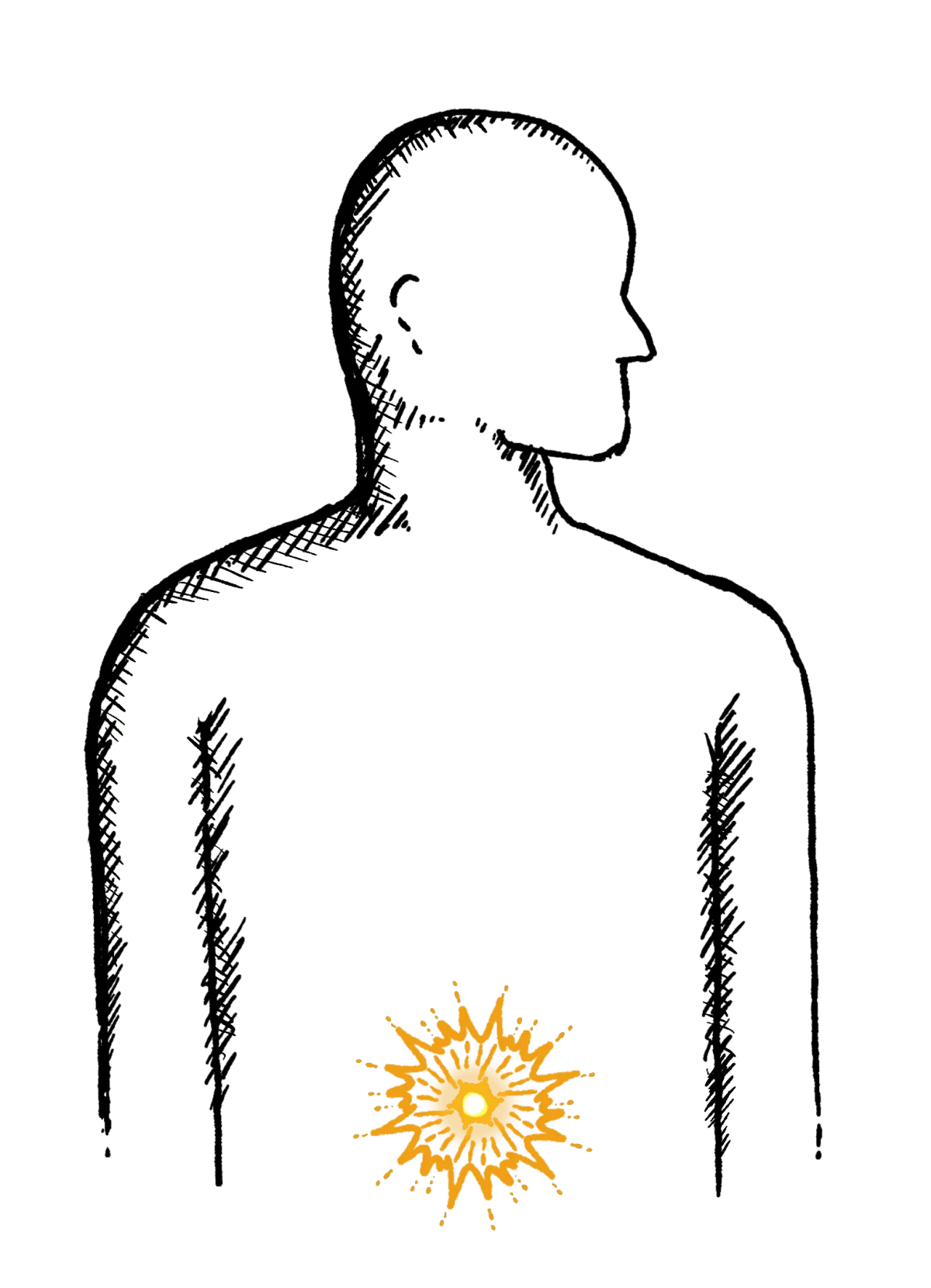
Loose or explosive stools, can’t get to a toilet in time
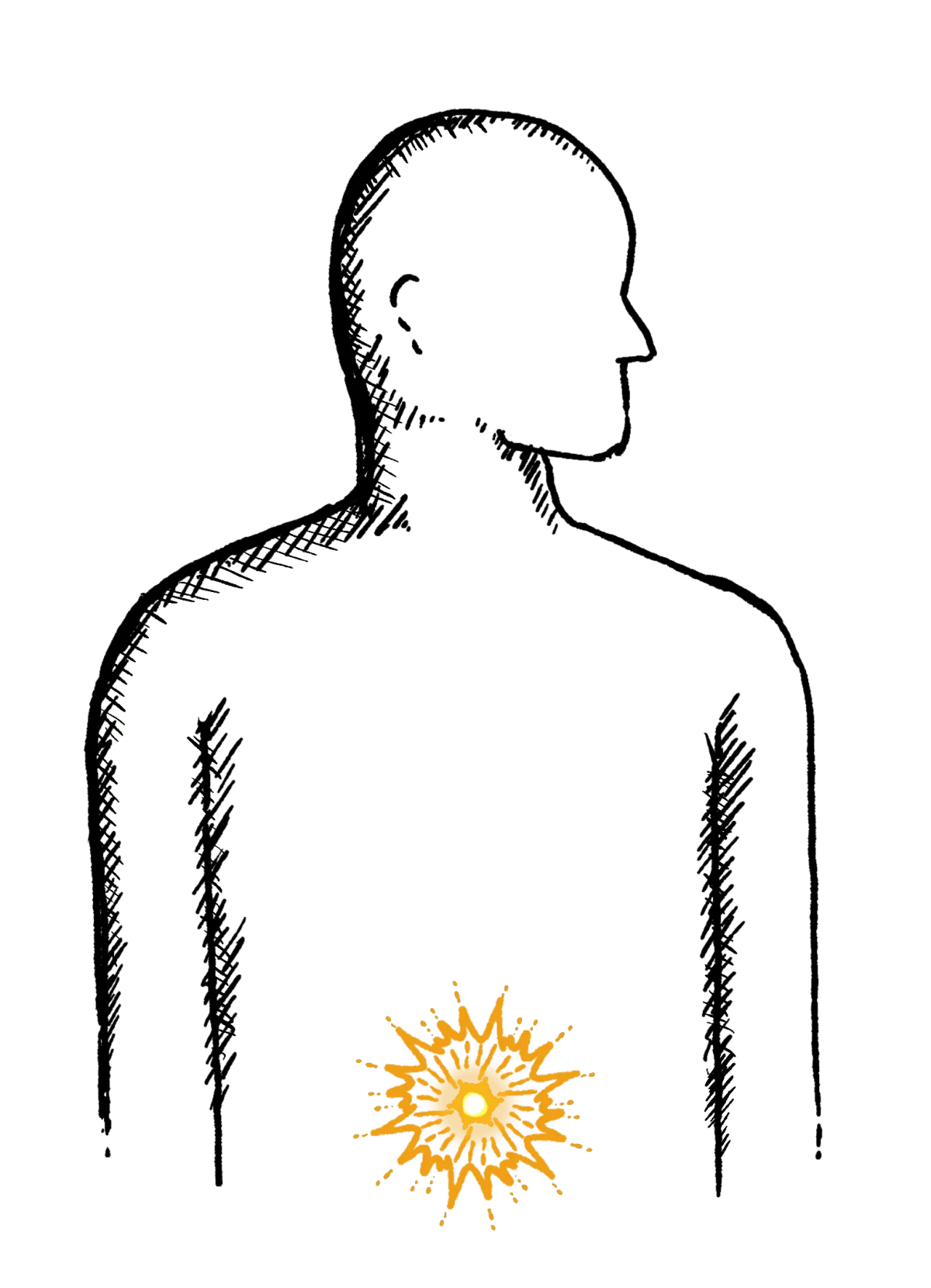
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

