Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

Can Stress Cause Acid Reflux?
Have you noticed that your acid reflux gets worse because of stress? You’re not imagining it. It’s a common question among people with acid reflux. Acid reflux, stress, and anxiety are closely related.
While stress itself cannot directly cause the condition, it can increase the risk of an acidity attack or make the symptoms of reflux feel more distressing. It’s not the only mechanism. Stress acts on your gut, leading to several gastrointestinal (GI) disorders.
So, does stress cause acid reflux? What’s the connection? And how can you treat acid reflux brought on by stress? Let’s find out.
Can Stress Cause Acid Reflux?
Yes and no.
Gastroesophageal reflux disease, or GERD, occurs when stomach acid repeatedly leaks into the food pipe (oesophagus), causing irritation. Common symptoms include heartburn, a hoarse voice, coughing, strange tastes, and bad breath.
So, how does stress cause acid reflux? Well, anxiety or stress works on almost every part of your body. Technically, stress itself doesn’t cause acid reflux. However, in people with predisposing factors, symptoms can worsen or exacerbate.
In a 2018 study, over 19,000 people with anxiety were investigated, noting a higher likelihood of experiencing GERD symptoms. Potential reasons include:
Reduces pressure in the lower oesophageal sphincter (LOS). Usually, your stomach acid cannot backflow due to the LOS, which prevents any leakage. However, if the pressure is reduced or the muscle relaxes, then the LOS can open. If you’ve eaten a large meal or have significant acid production, acid reflux can occur.
Increased stomach acid production. Perhaps the most obvious connection between stress and acid reflux is the rise in acid production. The more acid you produce, the greater the risk of reflux.
Rising pressure inside the stomach. When we feel stress, we often experience GI symptoms. That could include butterflies in the stomach, nausea, and even vomiting. This is because stress increases muscle tension, pushing acid from the stomach into the oesophagus.
Another 2024 study confirmed these findings. It found that acid reflux was 95% more likely to happen in those considered to have high levels of stress compared to those with low levels of stress.
Acid Reflux and Stress-Related Medications
It’s not just stress that causes acid reflux. Stress is often accompanied by other mental illnesses, such as anxiety or depression. If a person feels these conditions aren’t manageable on their own, then a doctor may prescribe medication.
Several of these medications can trigger acid reflux:
Antidepressants. Some selective serotonin reuptake inhibitors (SSRIs), like sertraline (Zoloft) and paroxetine (Paxil), can relax the oesophageal sphincter, which might lead to gastroesophageal reflux.
Anxiolytics (Anti-anxiety medications). Benzodiazepines such as diazepam (Valium) and lorazepam (Ativan) might relax the oesophageal sphincter, contributing to symptoms of acid reflux.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs). NSAIDs such as ibuprofen and aspirin, often used for stress-related symptoms like headaches and muscle pain, can irritate the stomach lining and increase acid production.
Beta-blockers. Such as propranolol, used for anxiety, migraine prevention, and other cardiovascular conditions related to stress, can potentially aggravate acid reflux symptoms.
It’s no surprise that people begin to associate acid reflux with stress. After all, these medications may only be taken during a stressful episode. It’s natural that a person connects the medication to the symptom. Speak to your doctor if you’re experiencing medication-related acid reflux.
How to Treat Acid Reflux from Stress
Dealing with acid reflux because of stress? The obvious solution is to resolve your stress levels. Often, people find a noticeable drop in their acidity attacks. Here are some tips:
Get more exercise. Regular exercise is a fantastic stress reliever, releasing stress-busting hormones.
Get enough sleep. The more sleep-deprived we are, the worse our stress levels. Ensure you get 7-8 hours per night – add a few extra pillows or lying on your left-hand side to prevent acid reflux during the night.
Practice yoga or mindfulness. Activities like yoga, tai chi, and mindfulness can lower your stress levels. Alternatively, pick a calming activity you enjoy.
Eat healthily. It’s tempting when we’re stressed to binge on junk food. However, that will only exacerbate your symptoms. Avoid fatty, spicy foods that trigger reflux.
Getting Diagnosed with Acid Reflux
Do these acid reflux signs and symptoms look familiar? If so, it’s worth getting tested. Here at The Functional Gut Clinic, we offer several testing options for people with acid reflux. These include 24-hour reflux testing to confirm the presence of acid in your oesophagus or oesophageal manometry, which measures if your LOS is working properly.
We provide you with a comprehensive explanation of the results and advise you on the next step. With years of experience, we’re the best option for reflux testing. Confirm your GERD symptoms with our help. Contact us today to learn more.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
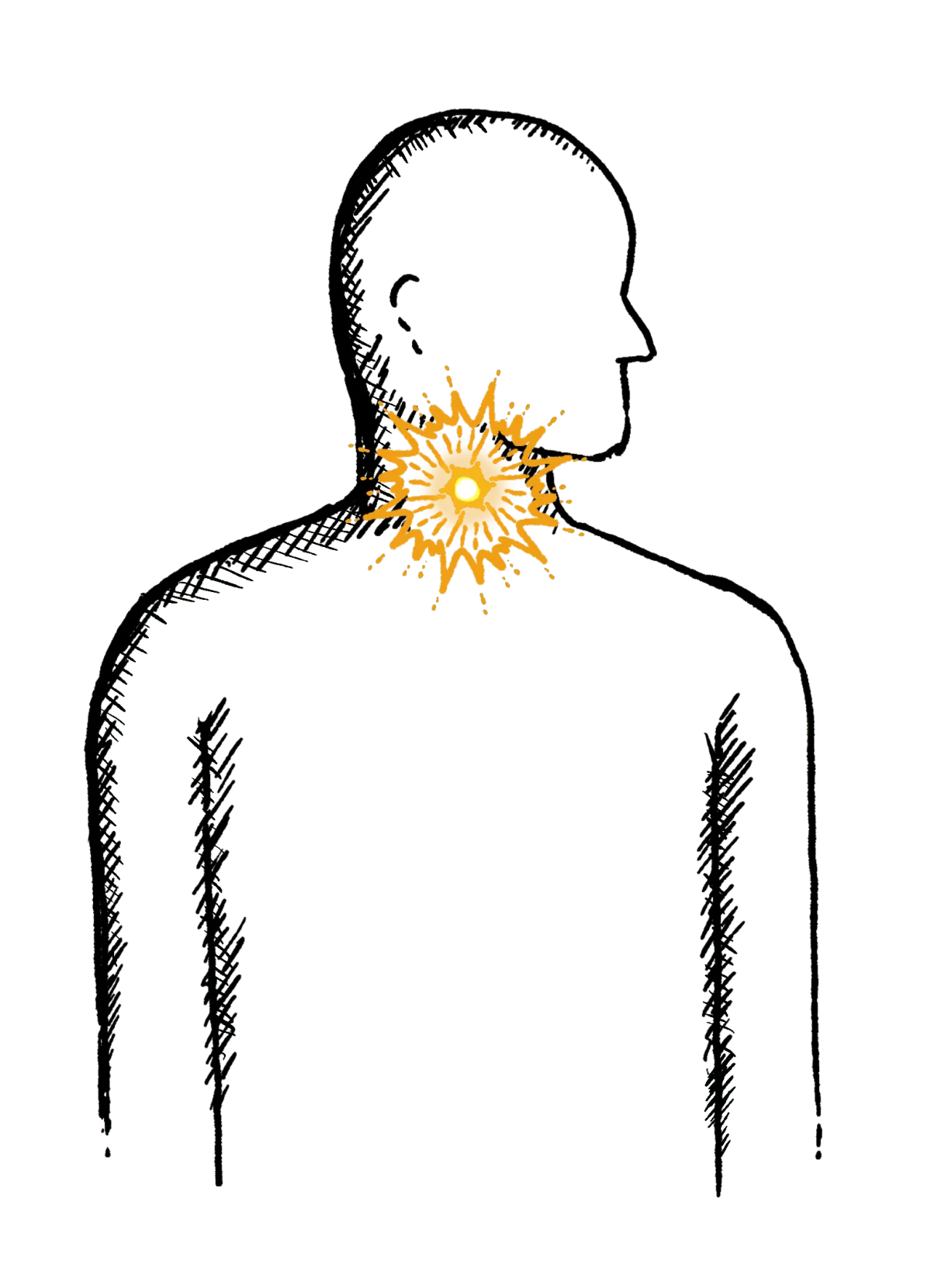
Reflux
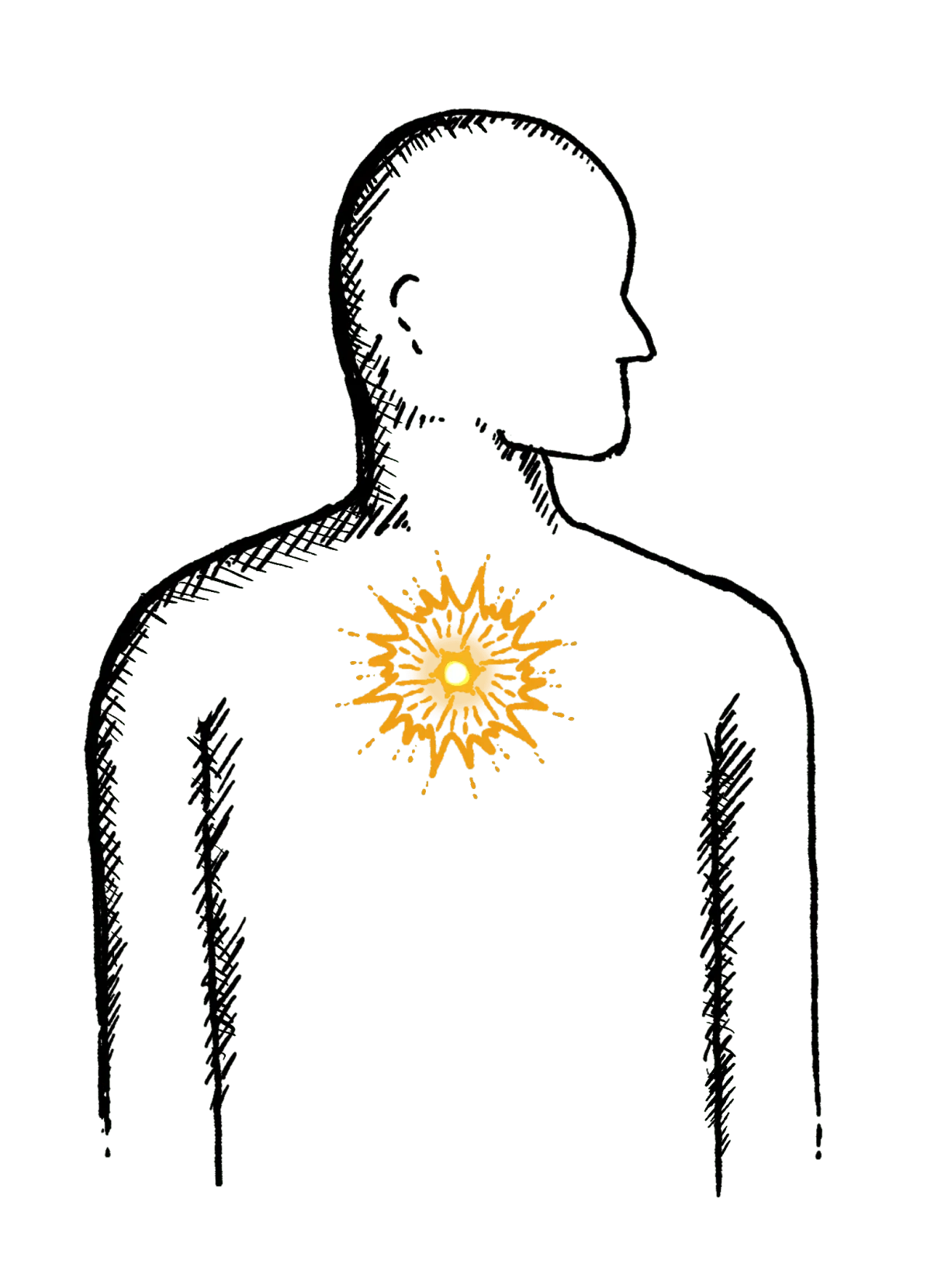
Burning mid-chest, worse when bending or lying down
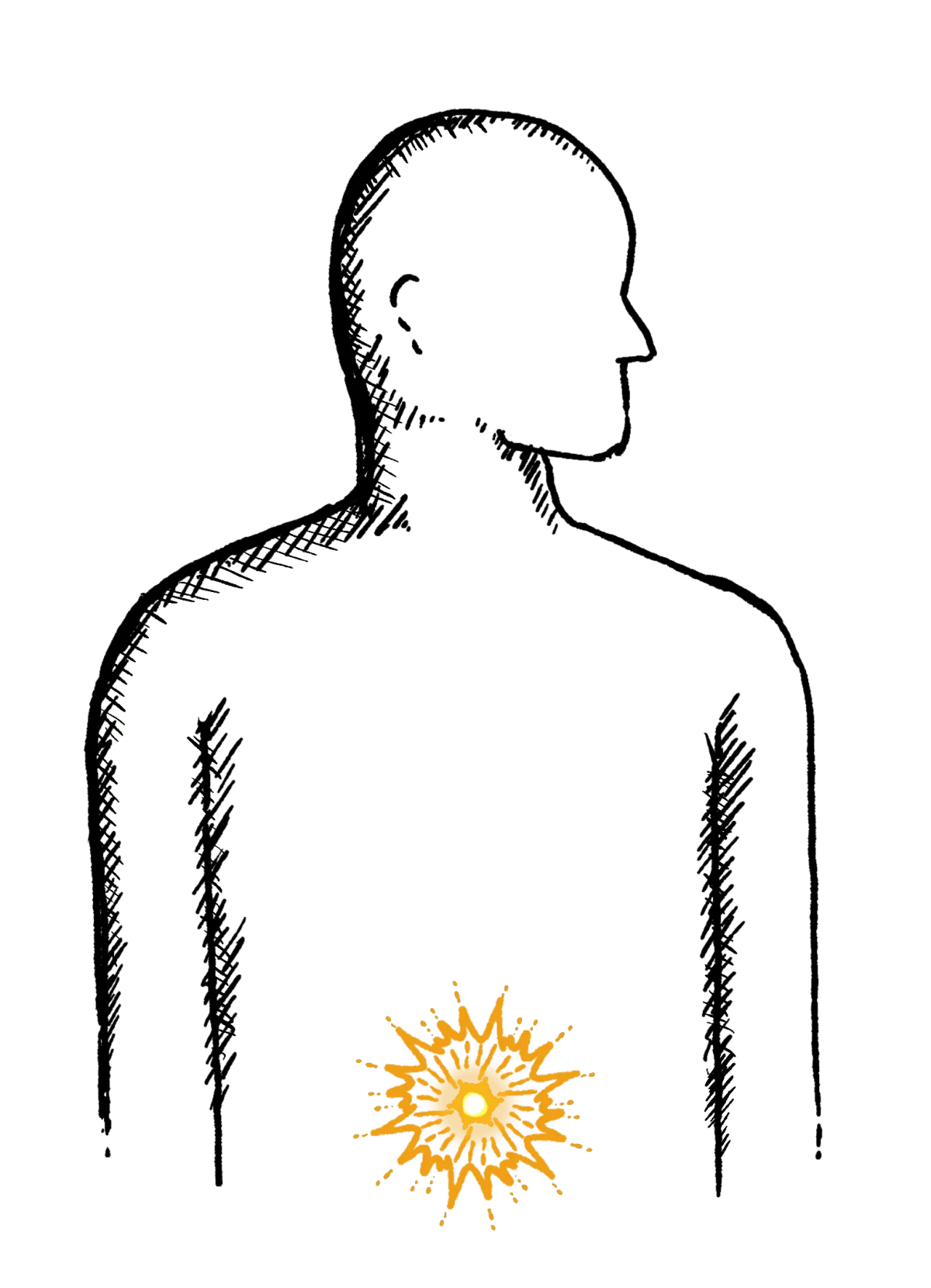
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
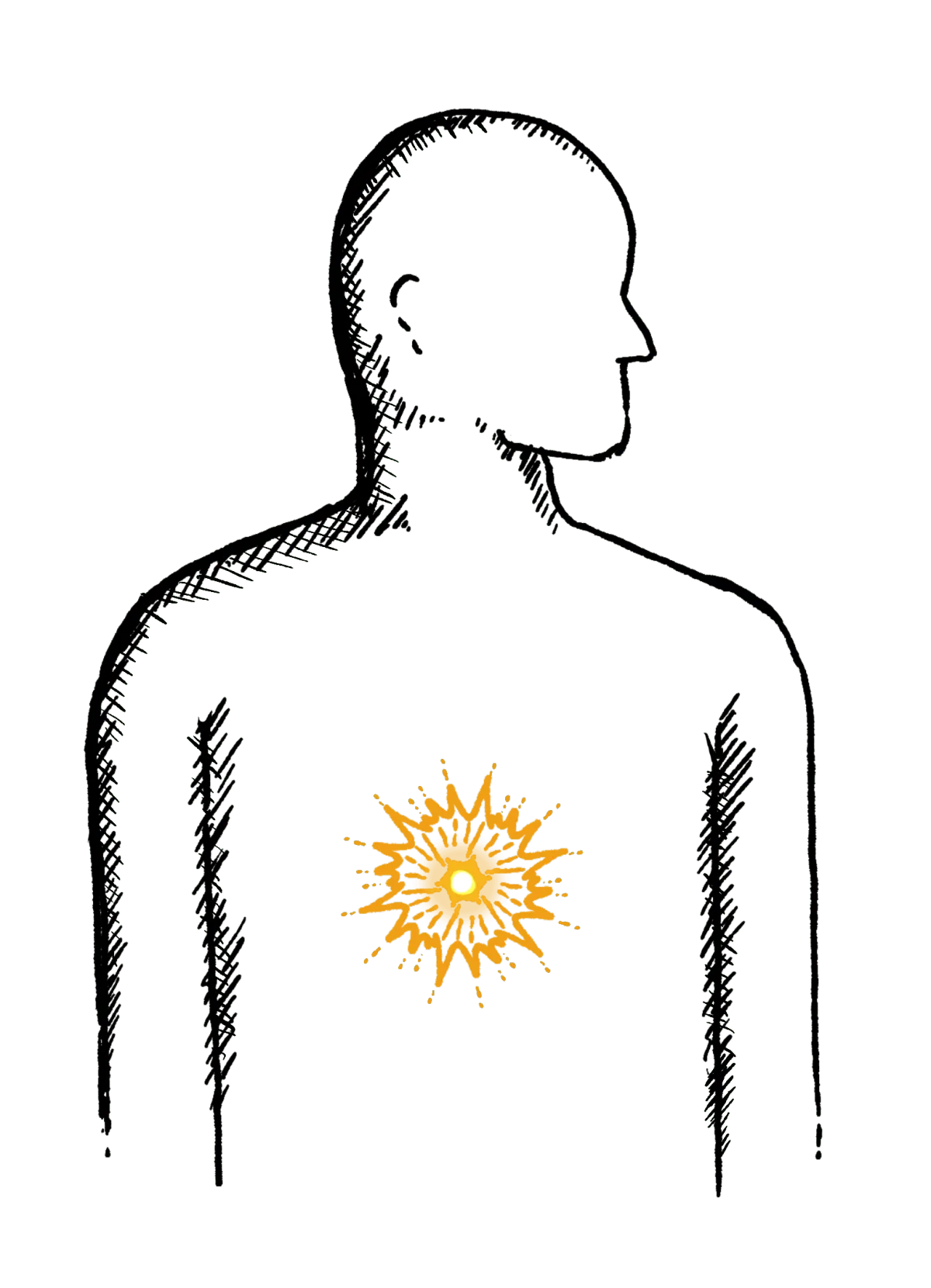
Heartburn
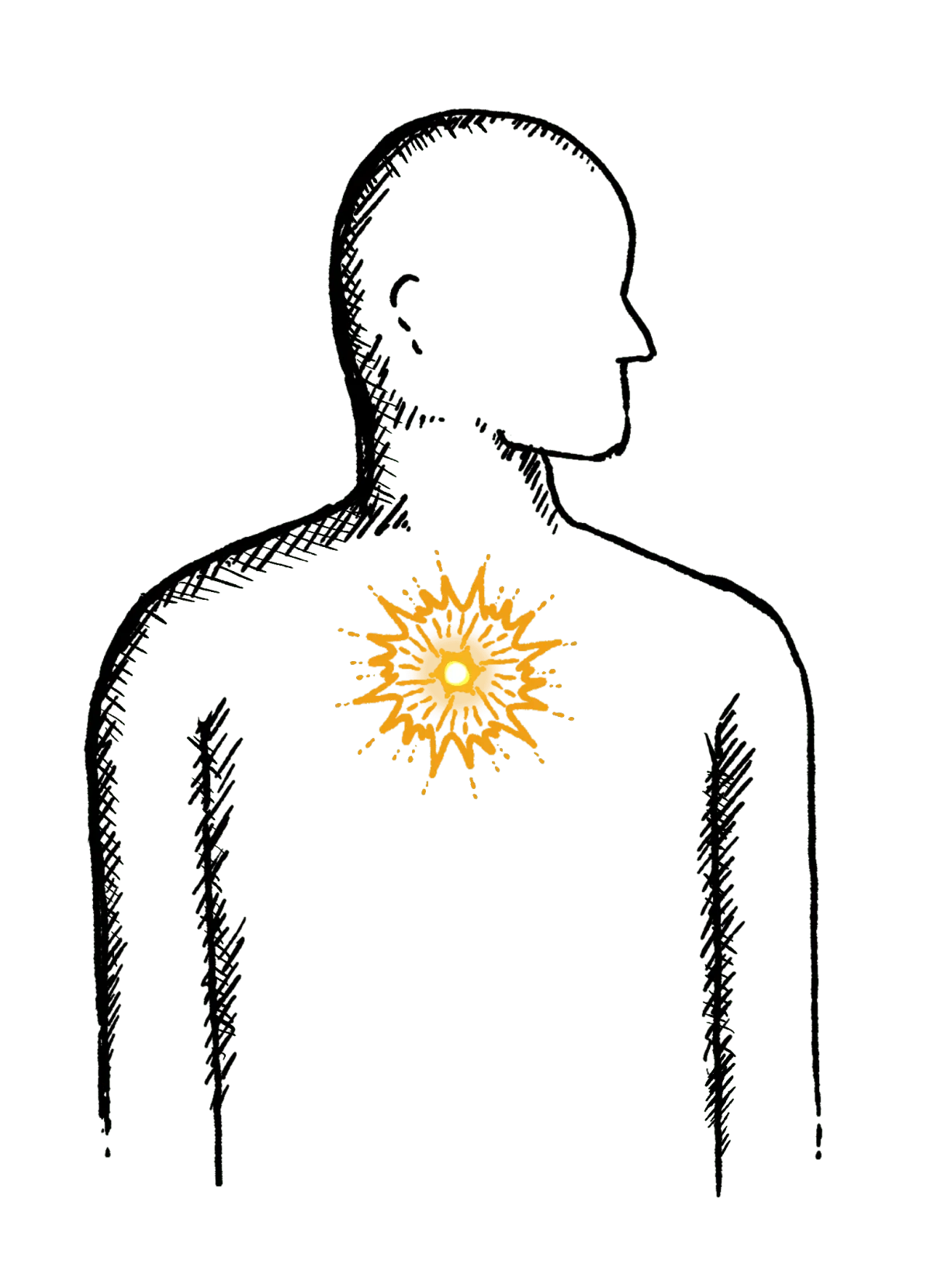
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
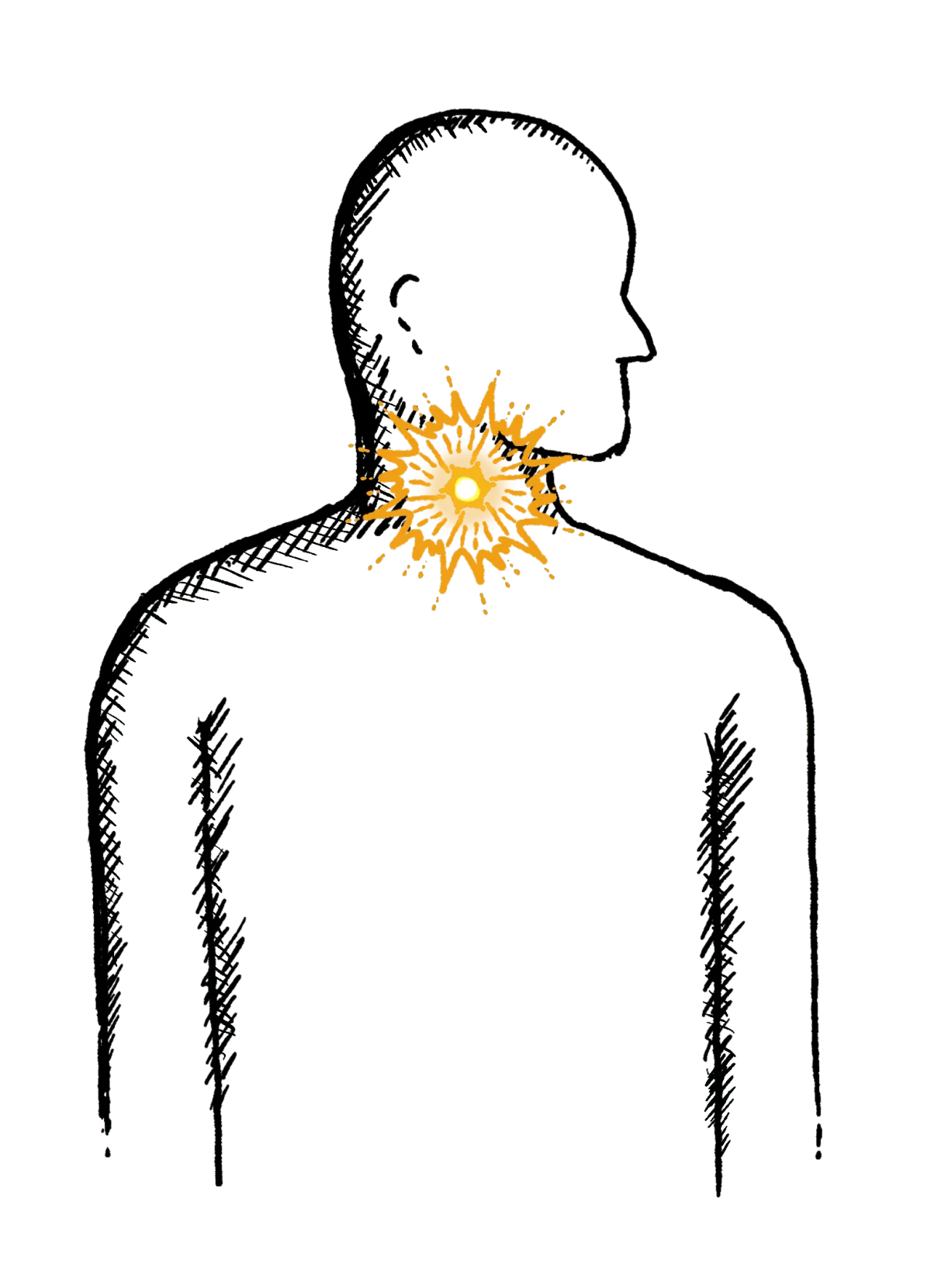
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Diarrhoea
Loose or explosive stools, can’t get to a toilet in time
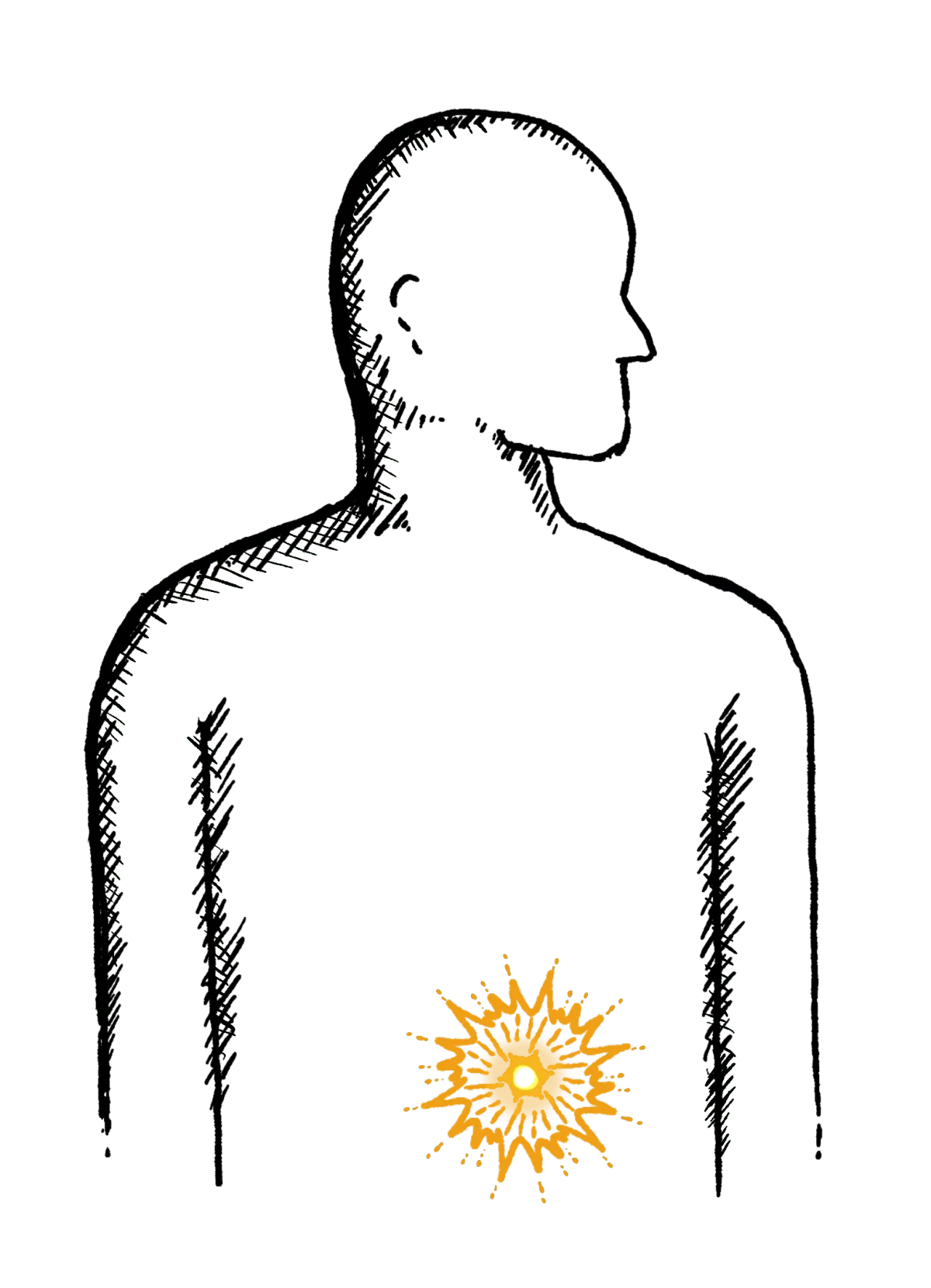
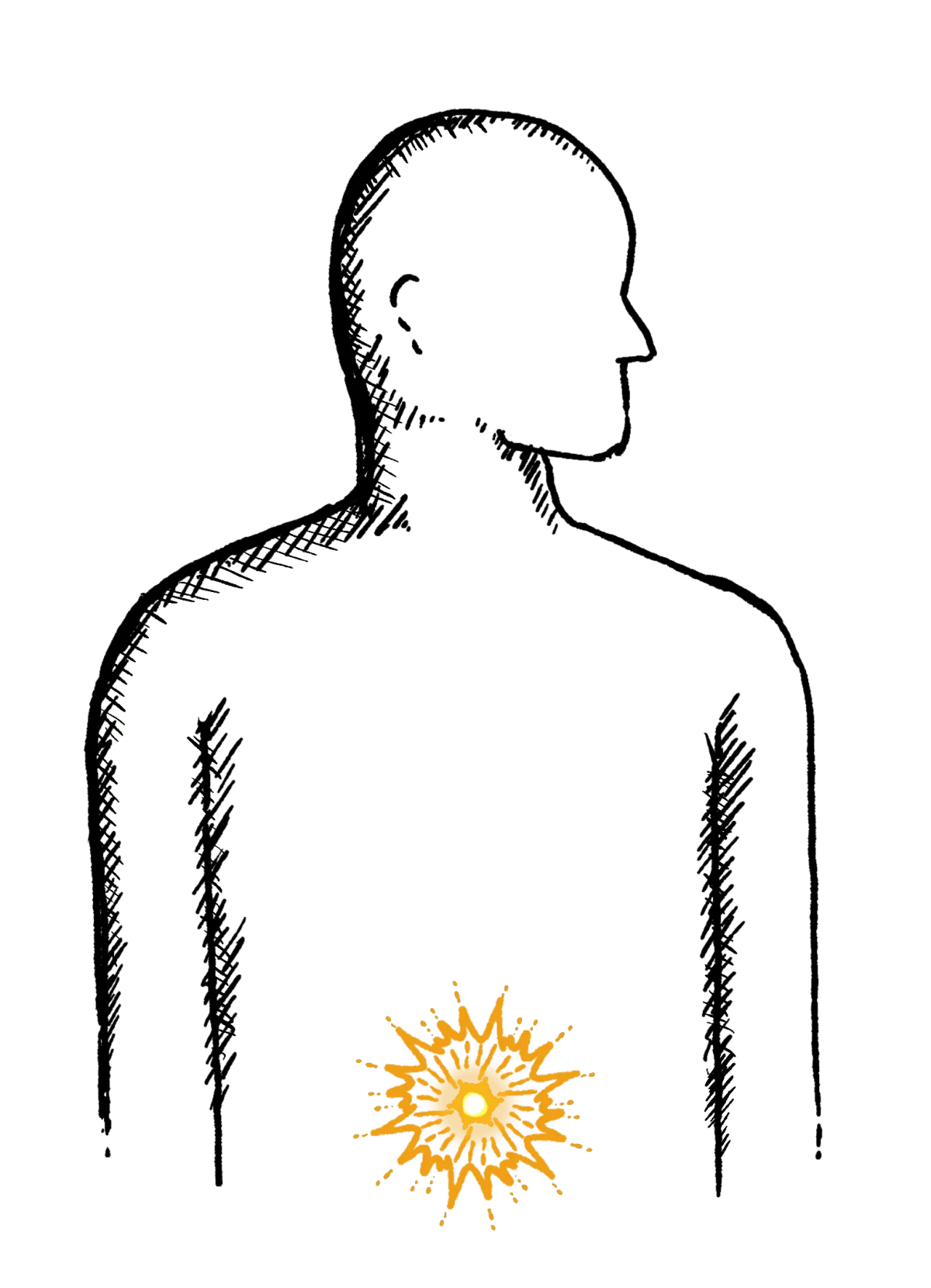
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

