Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

Sleep struggles? How to help night-time reflux
Lots of people find that their reflux is particularly bad during the night, which makes sense because when we are lying down, gravity isn’t there to help the acid from our stomach stay in our stomach. Leading to all sorts of burdensome symptoms like burning, chest pain, acid taste and cough.
There are lots of little techniques you can use to try and reduce the amount of reflux you get at night. Not all of these will work for everyone, and you may have already tried and tested these methods yourself. But with that here are our top tips for reducing night-time reflux which don’t include medications:
1. Chewing gum – some research has shown that chewing sugar-free gum could reduce reflux due to the chewing action causing increased swallowing, promoting acid clearance in the oesophagus. The action of chewing gum can also stimulate gastric juice secretion, boosting digestion of food contents, and reducing stomach contents which may otherwise increase reflux risk.
2. Sleeping on your left-hand side – due to the anatomy of the stomach and the way the opening sits, lying on your left-hand side can ensure the opening of the stomach is upright, allowing gravity to help keep stomach contents down and avoid anything refluxing up.
3. Wait 3-4hrs after eating before going to bed – having lots in your stomach increases abdominal pressure and the likelihood of reflux. Leaving a sufficient amount of time for digestion to occur and stomach contents to empty means there is less available in the stomach to reflux up. Additionally, less acid for digestion will be being produced and so, less acid available to cause reflux.
4. Avoid trigger foods – if you have known trigger foods such as spicy foods and fatty foods, then it is particularly important that you avoid these at night as you do not have the advantages of being upright and going about normal daily activities, such as a light stroll, to help prevent reflux from happening.
5. Have a light dinner – eating a large meal, or even just a meal that is full of spice or fatty foods, can increase the risk of reflux at night. Try having a smaller meal to prevent the pressure in your stomach to increase due to the larger volume in it. Additionally, try to avoid meals high in fat, as this can delay digestion, causing food to remain in your stomach for a longer amount of time, increasing the likelihood of food and acid moving up into your oesophagus.
6. Limit liquids before bed – consuming a lot of liquids, just like eating a large meal, can increase the pressure in your stomach and increase the risk of contents moving up into the oesophagus and causing reflux. Aim to consume enough during the day to avoid downing pints of water in the evening
7. An extra pillow – further helping gravity do it’s thing, sleeping with your head upright allows any reflux at night to stay down.
8. Avoid alcohol in the evening – alcohol is a common culprit for many people when it comes to reflux. This makes sense as some research has shown that alcohol may cause the ring of muscle at the top of our stomach stopping stomach contents refluxing up to relax.
9. Avoid strenuous exercising before going to bed – high intensity and strenuous exercise can may increase the risk of reflux because, as with eating a large meal, these types of workouts can increase abdominal pressure which helps push things out of the stomach and into the oesophagus.
10. Practice relaxation techniques before bed – research has shown that practicing relaxation techniques such as diaphragmatic breathing may help reduce reflux and it’s symptoms which could be particularly beneficial if you suffer from night-time reflux as it not only helps with reflux but gets you relaxed and ready for bed, hopefully improving your overall sleep.
The bottom line...
There are plenty of techniques you can apply to your evening routine in order to help prevent that unpleasant night-time reflux from happening, which don’t include medications.
If you have given these a try, and you still find your reflux ruining your night and sleep, then please seek further medical advice from your consultant. They could help you look for further treatment plans and potentially refer you for further diagnostic testing to assess your reflux and its causes.
References
The effect of chewing sugar-free gum on gastro-esophageal reflux - PubMed
Walking and chewing reduce postprandial acid reflux - PubMed
The effect of sleep positional therapy on nocturnal gastroesophageal reflux measured by esophageal pH-impedance monitoring - PubMed
Lifestyle Intervention in Gastroesophageal Reflux Disease - PubMed
Gastroesophageal Reflux Disease (GERD): Highlighting Diagnosis, Treatment, and Lifestyle Changes - PMC
The role of lifestyle changes in gastroesophageal reflux diseases treatment - PubMed
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
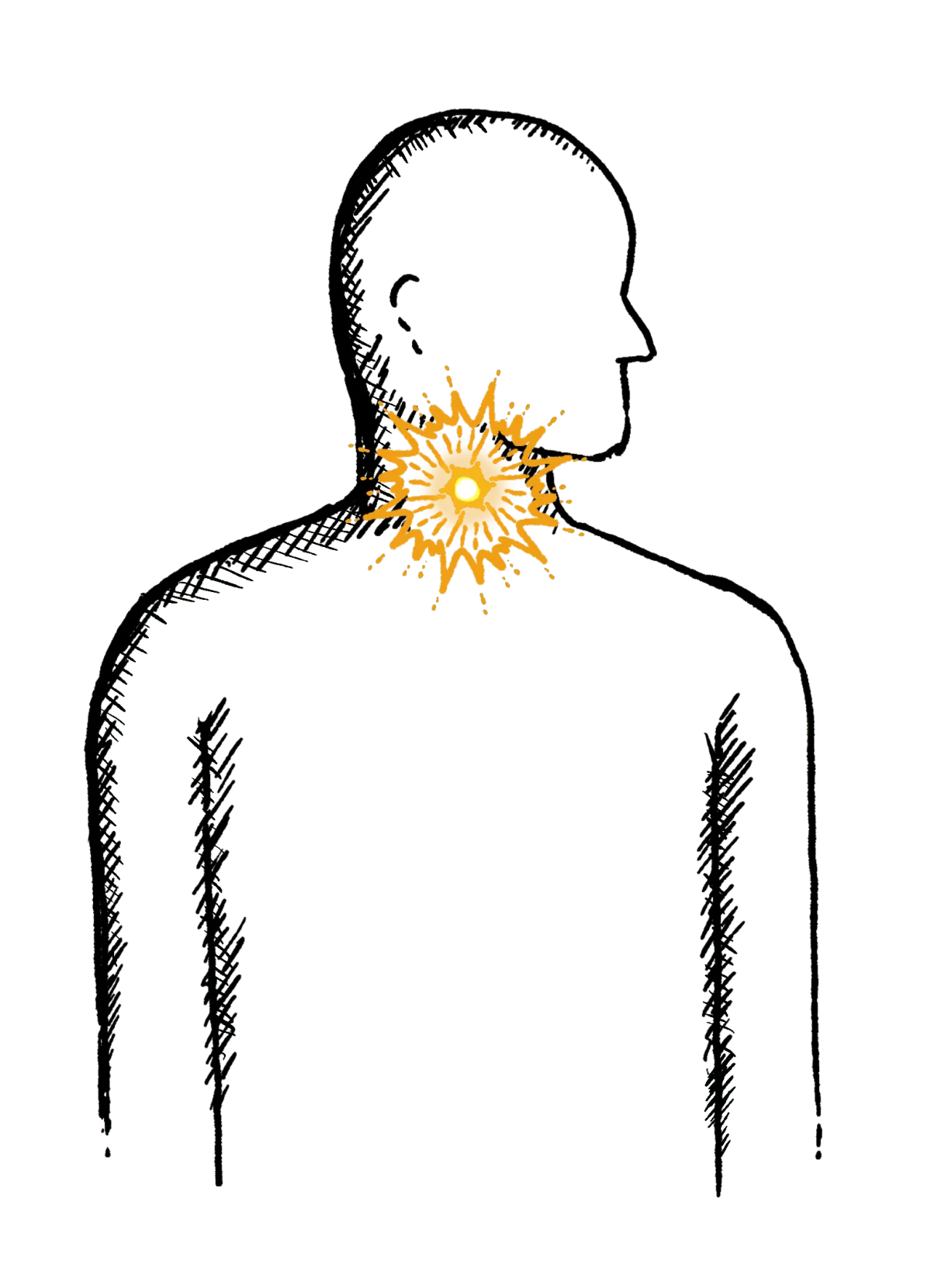
Reflux
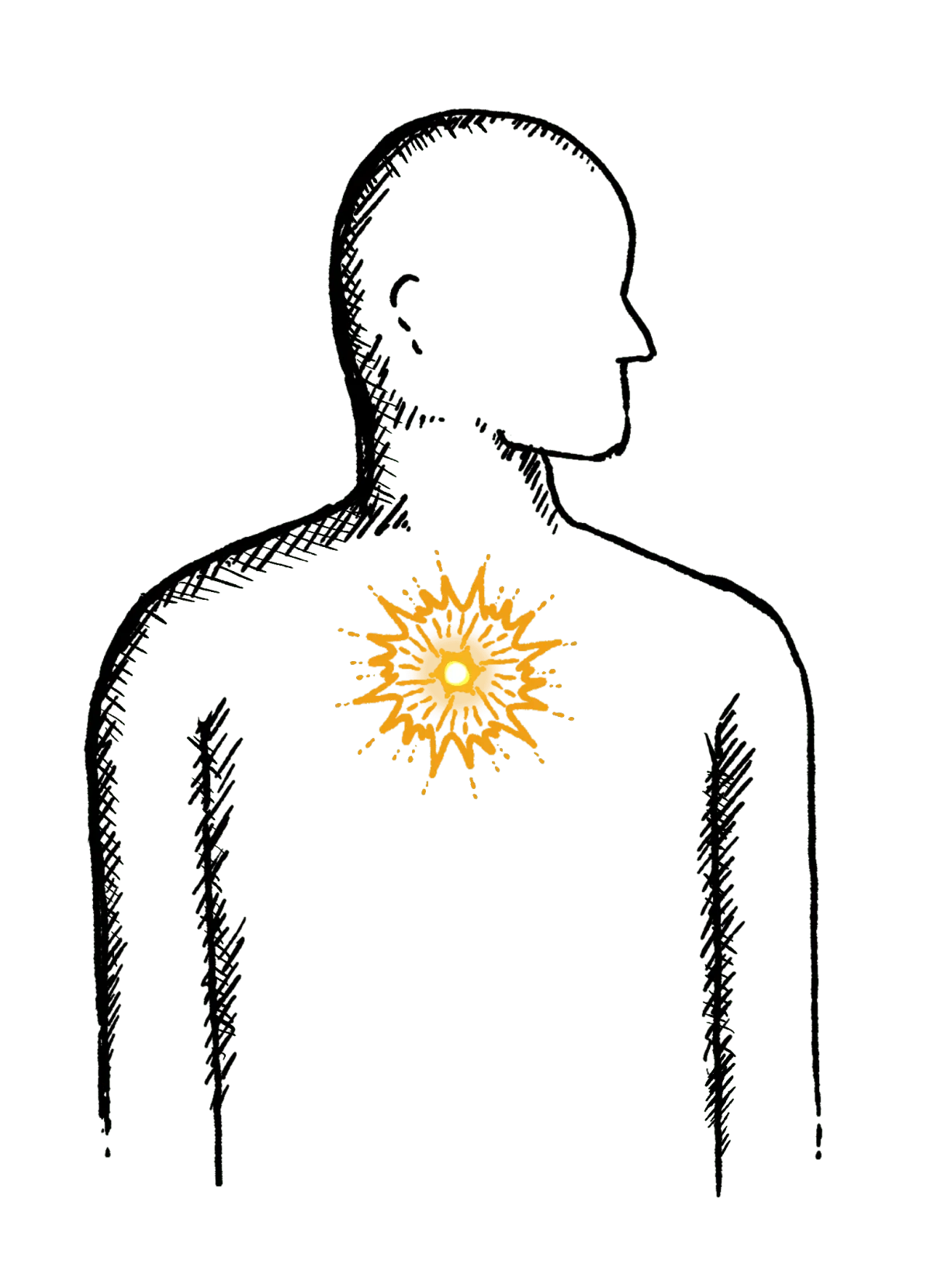
Burning mid-chest, worse when bending or lying down
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
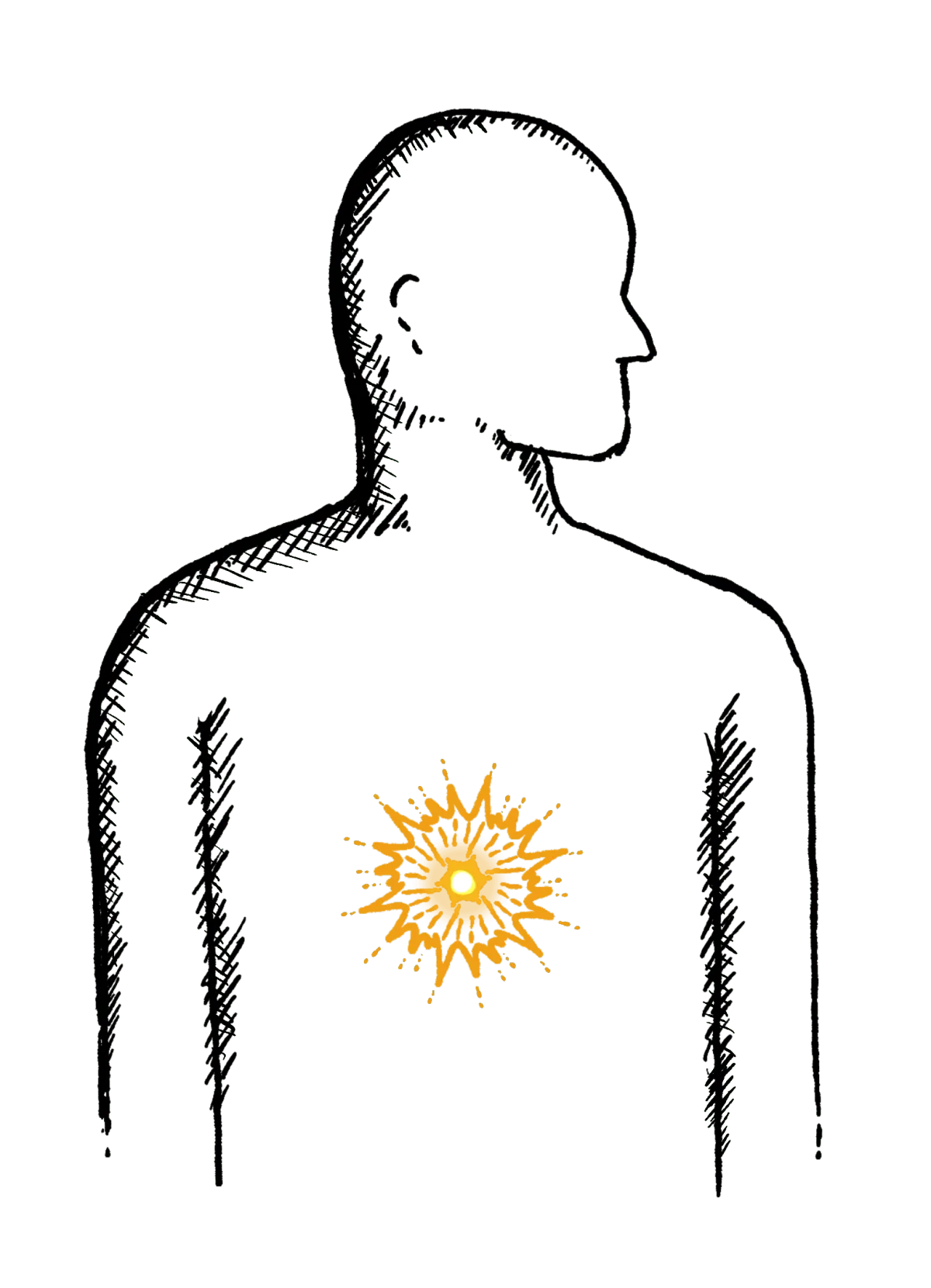
Heartburn
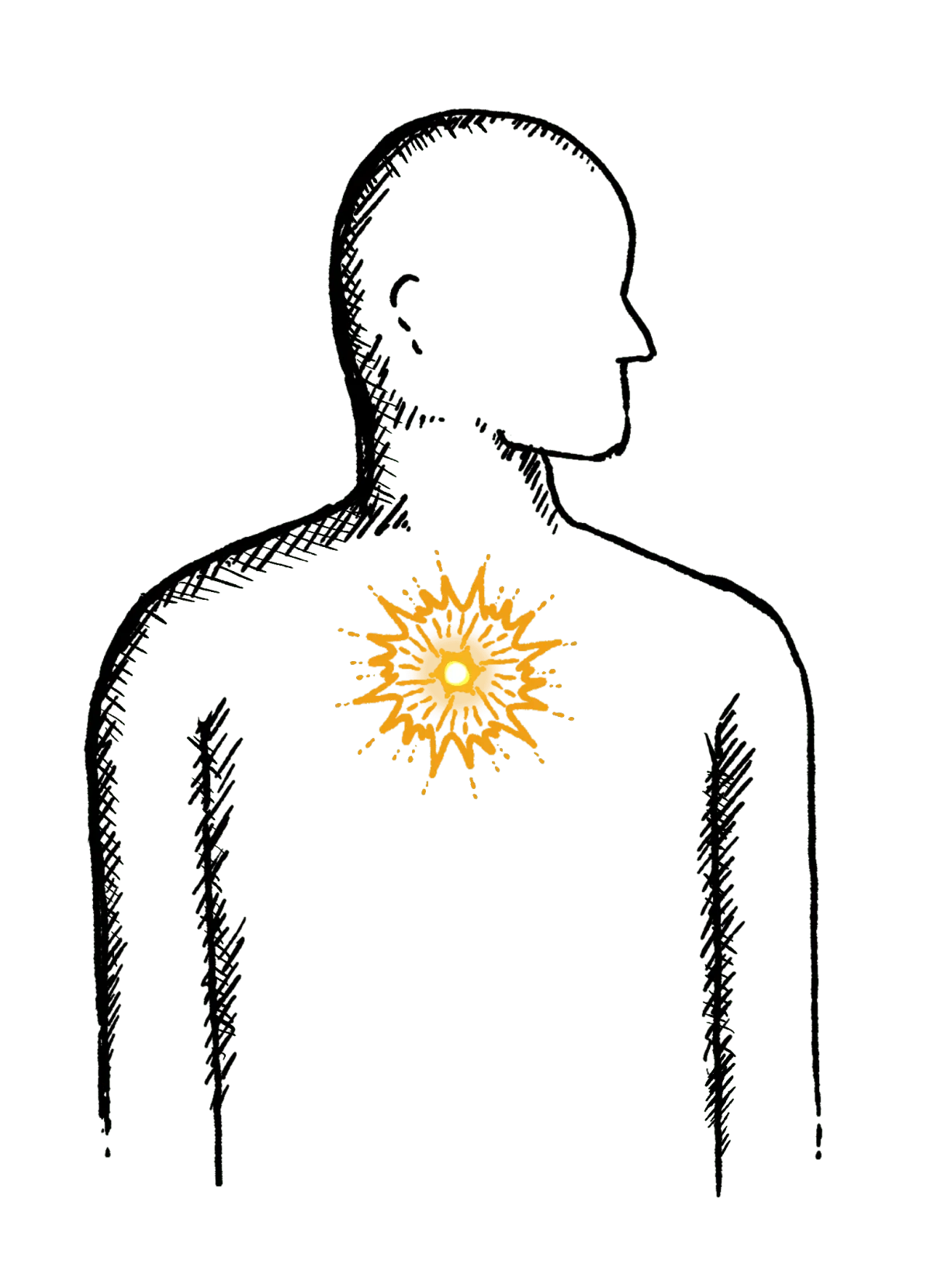
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
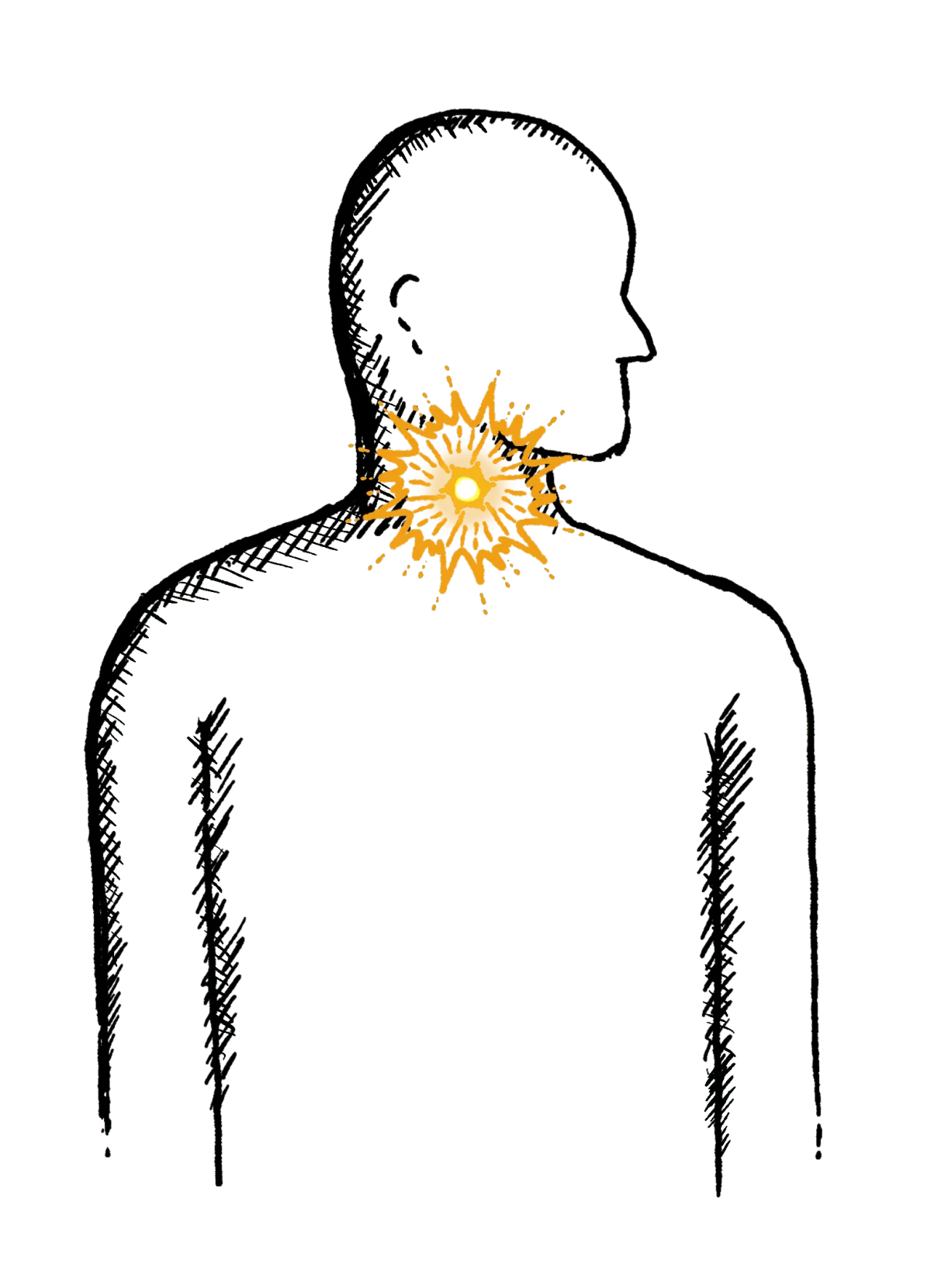
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Diarrhoea
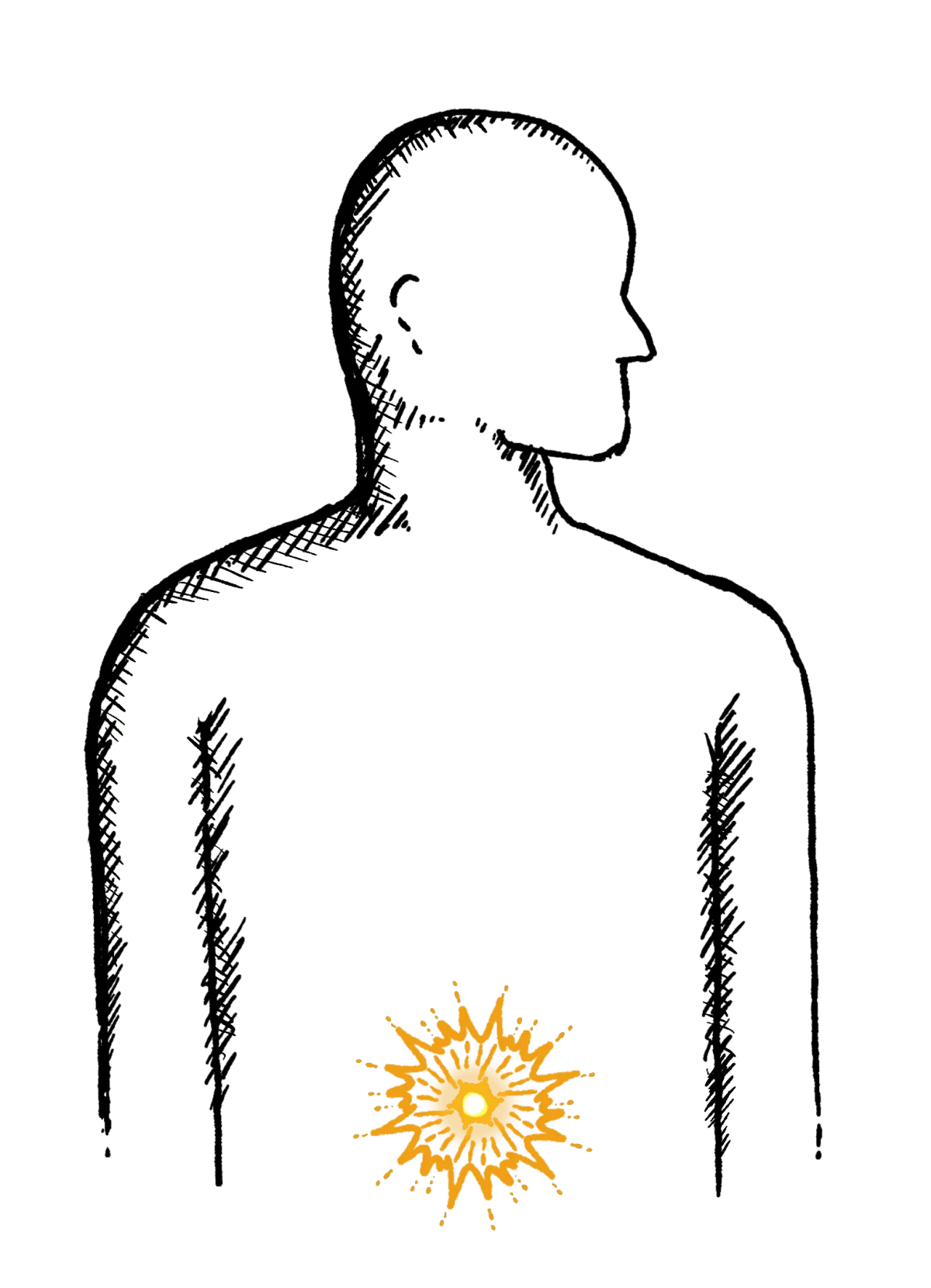
Loose or explosive stools, can’t get to a toilet in time
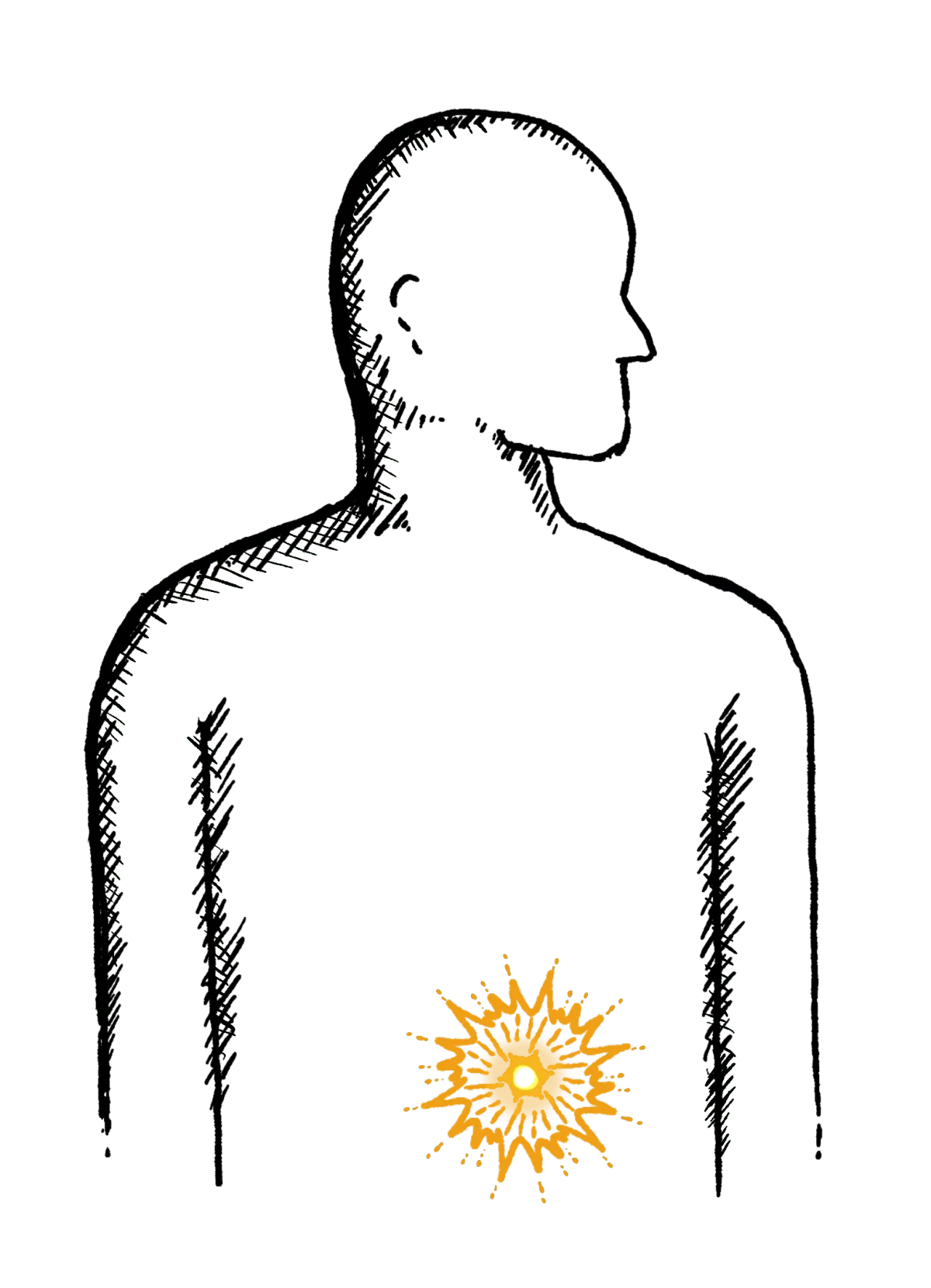
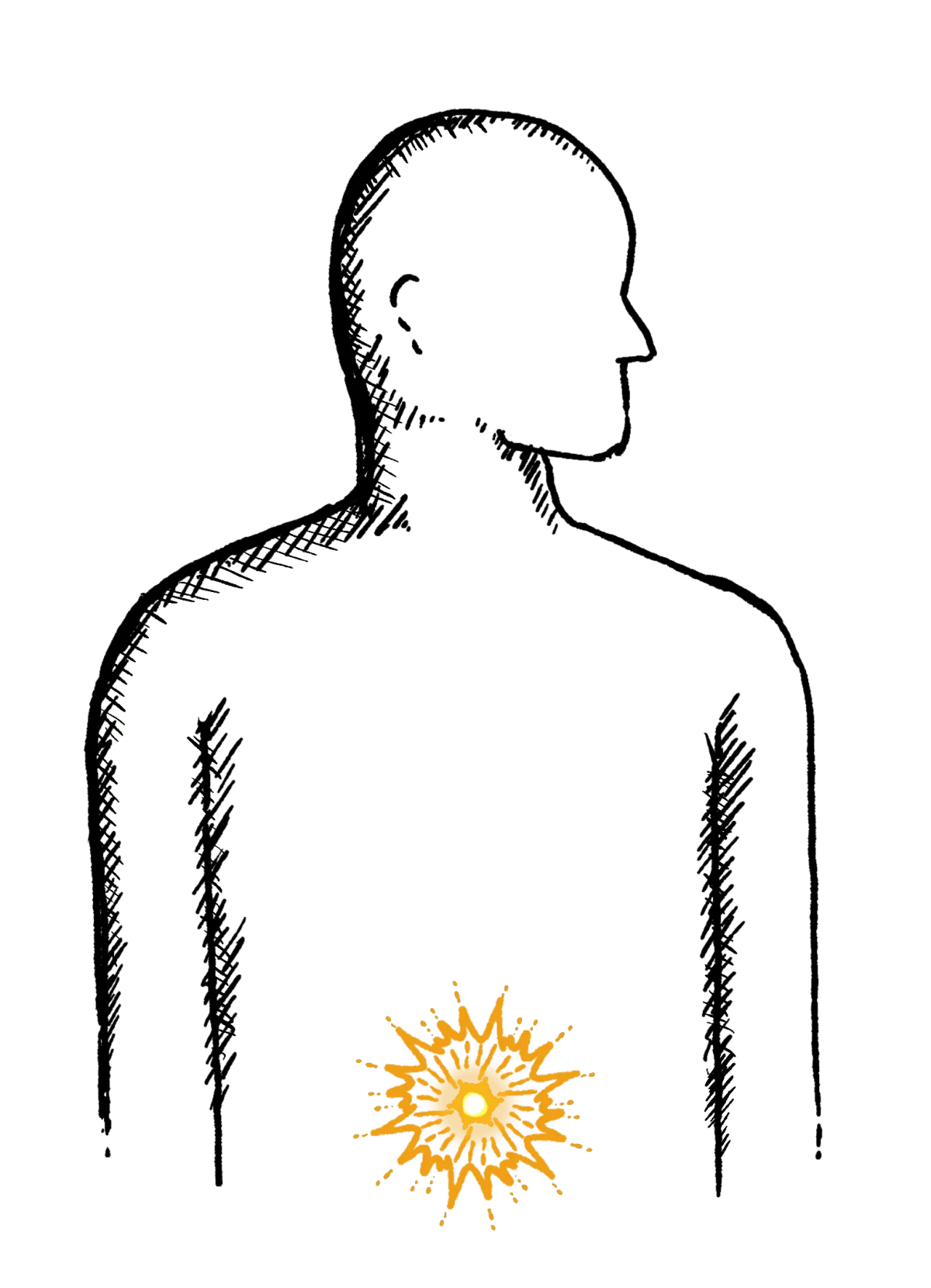
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

