Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY



What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

Understanding Your IBS: Treatment Options and Clinical Support
Living with Irritable Bowel Syndrome (IBS) can be frustrating, especially when typical strategies haven’t helped. If you're struggling with persistent symptoms such as abdominal pain, bloating, constipation or diarrhoea, there are several clinical and lifestyle options you can explore.
Below, we've outlined some of the most widely used and evidence-based approaches to managing IBS symptoms. Each person's experience with IBS is unique, so the best treatment approach for you may involve combining multiple strategies tailored to your individual needs.
If you’d like to learn more about clinical support options or discuss a personalised care plan, request our free IBS Support Factsheet (sent via email) or get in touch with our clinical team to explore your next steps.
1. Nutrition Interventions
Dietary adjustments are often a first-line strategy for managing IBS, with good evidence supporting their effectiveness. Working with a specialist gut dietitian can be particularly helpful to guide you through approaches such as:
Low FODMAP diet: Temporarily restricting specific fermentable carbohydrates that commonly trigger IBS symptoms like bloating, gas and abdominal pain, before reintroducing to find your tolerance level. This should only be done under the guidance of a specialist FODMAP-trained dietitian.
Identifying personal food triggers: Often utilising food diaries and taking a structured approach to find and manage specific food sensitivities.
2. Lifestyle Support
Stress and anxiety frequently worsen IBS symptoms, making gut-focused psychological therapies highly effective additions to your management plan. These approaches include:
Mindfulness and stress management techniques: Can help calm the gut-brain axis and reduce symptom severity.
Cognitive Behavioural Therapy (CBT): Helps you manage the psychological factors influencing your symptoms.
Gut-directed hypnotherapy: Reduces gut sensitivity and improves symptom control in many IBS sufferers.
Regular gentle exercise and consistent sleep patterns can also significantly improve IBS symptoms.
3. Probiotics and Supplements
Some individuals with IBS find relief from certain probiotics (beneficial bacteria that aim to support gut health). Although research results vary between probiotic strains and individuals, certain probiotics can help manage symptoms, such as bloating and abdominal discomfort.
Additionally, evidence-based supplements such as peppermint oil capsules have been shown in clinical trials to ease gut spasms and reduce pain in IBS.
4. Prescription Medications and Medical Support
Your clinician may consider prescription medications to manage more persistent or severe symptoms. The following medications are commonly recommended:
Antispasmodics (e.g., mebeverine, hyoscine): Used to relieve abdominal cramps and spasms.
Laxatives or prokinetics: For constipation-predominant IBS (IBS-C) to help improve bowel regularity.
Anti-diarrhoeals: For diarrhoea-predominant IBS (IBS-D) to slow gut transit and improve stool consistency.
Non-absorbable antibiotics (such as rifaximin): Sometimes prescribed if bacterial overgrowth (SIBO) is suspected.
Low-dose antidepressants (such as amitriptyline): May help ease chronic abdominal pain and improve gut-brain communication.
5. Advanced Testing and Specialist Assessments
For complex, persistent IBS cases where symptoms remain unresolved despite standard approaches, advanced diagnostic testing can help identify underlying causes or co-existing conditions. At The Functional Gut Clinic, we offer a range of clinical testing and evidence-based options to help investigate your symptoms and support you in managing IBS more effectively.
We understand that no two experiences of IBS are the same, which is why individualised assessment and management are key. Diagnostic testing includes:
Breath tests: For conditions like Small Intestinal Bacterial Overgrowth (SIBO) and carbohydrate intolerances (e.g., lactose).
Stool analyses: To assess gut inflammation, microbiome composition, and exclude certain infections.
Gut motility and transit studies: Evaluating how well food moves through your digestive tract, which can significantly influence symptoms.
6. Emerging Microbiome Therapies
Increasing research into the gut microbiome has prompted scientists and clinicians to explore new investigational therapies focused on modifying gut bacterial composition. Find out more in our Understanding FMT blog article.
If you're interested in finding out more about specialist clinical assessments and whether advanced microbiome-focused approaches could be suitable for your case, request our free IBS Support Factsheet or get in touch with our team.
More support for IBS patients
At The Functional Gut Clinic, we specialise in supporting patients with chronic, hard-to-manage IBS symptoms. We offer comprehensive clinical assessments, specialist diagnostic testing and tailored management plans to help you regain control of your gut health.
If you'd like to find out more about advanced support options, including specialist microbiome approaches, request your free IBS Support Factsheet below:
Disclaimer: This article is intended for informational and educational purposes only, and does not constitute medical advice or offer of treatment. Always consult a healthcare professional before beginning new treatments or interventions.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
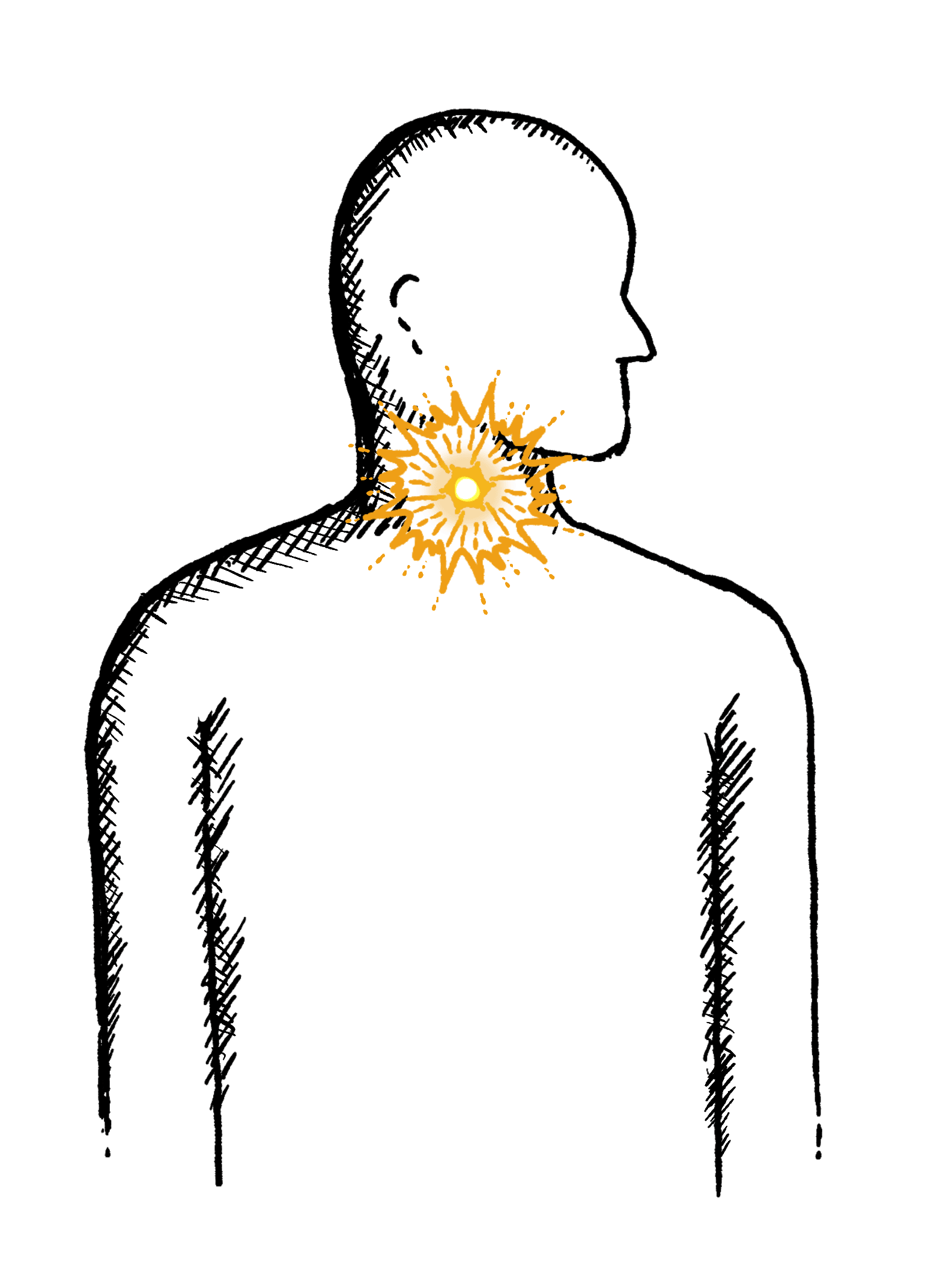
Reflux
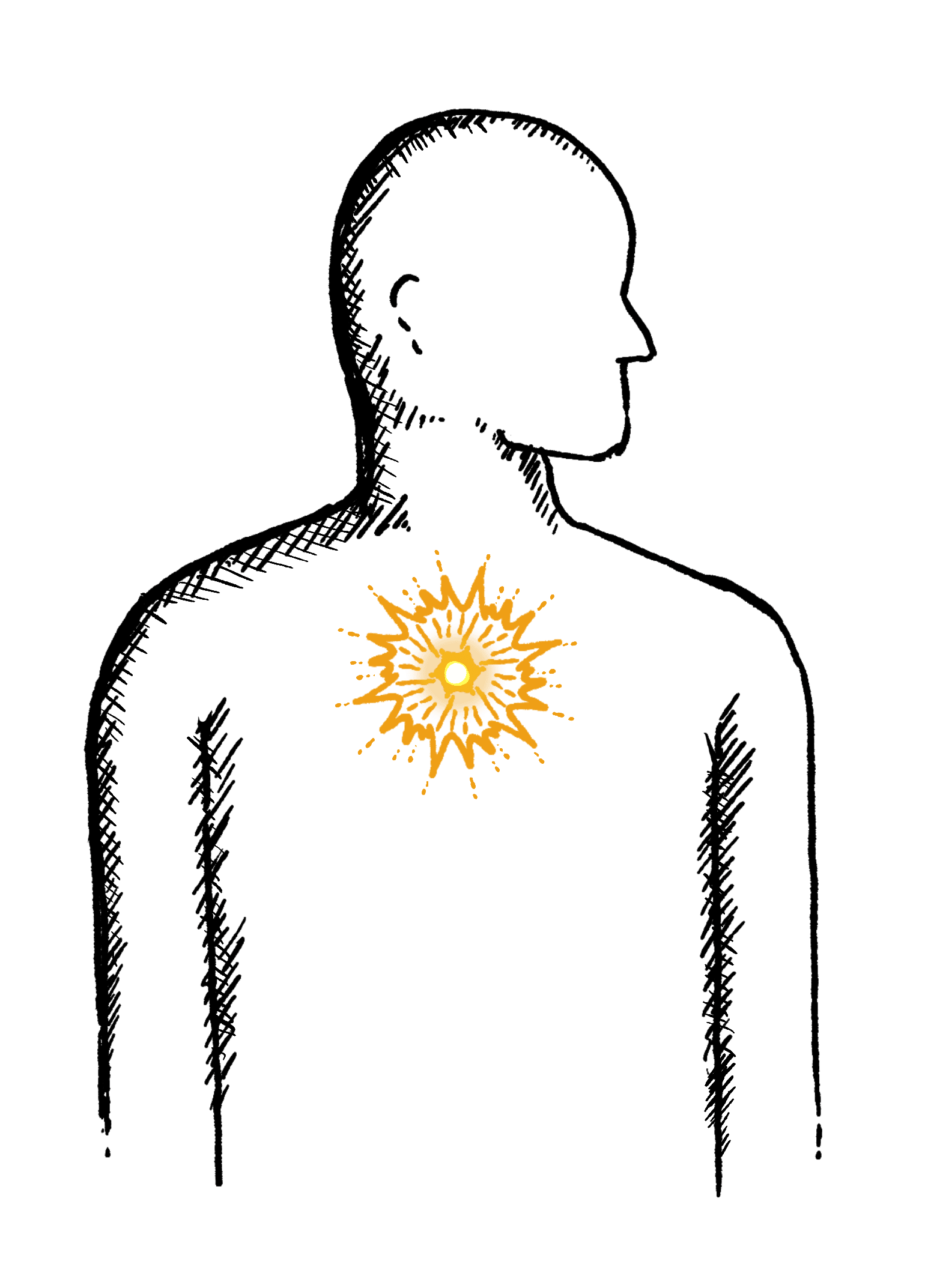
Burning mid-chest, worse when bending or lying down
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
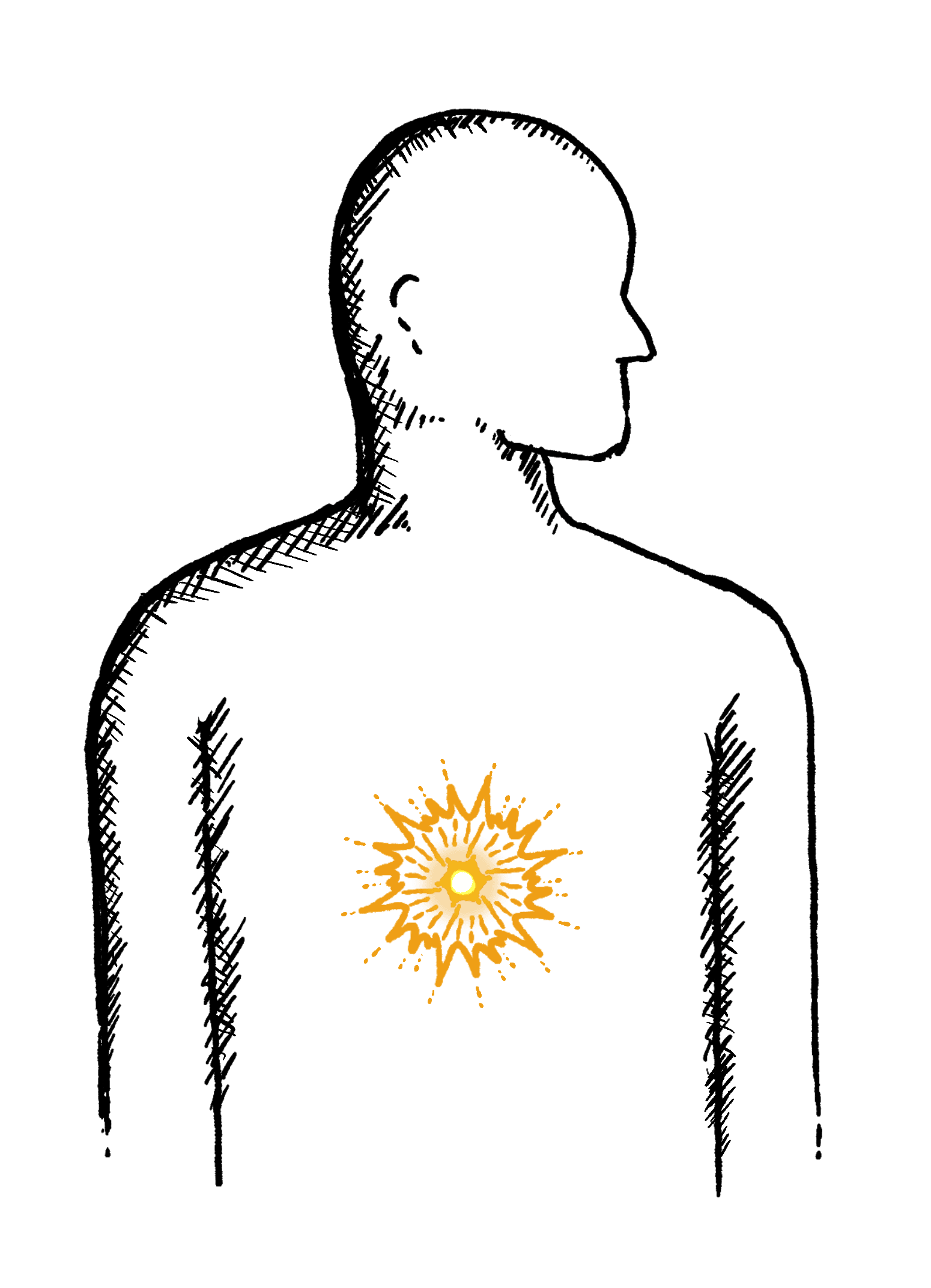
Heartburn
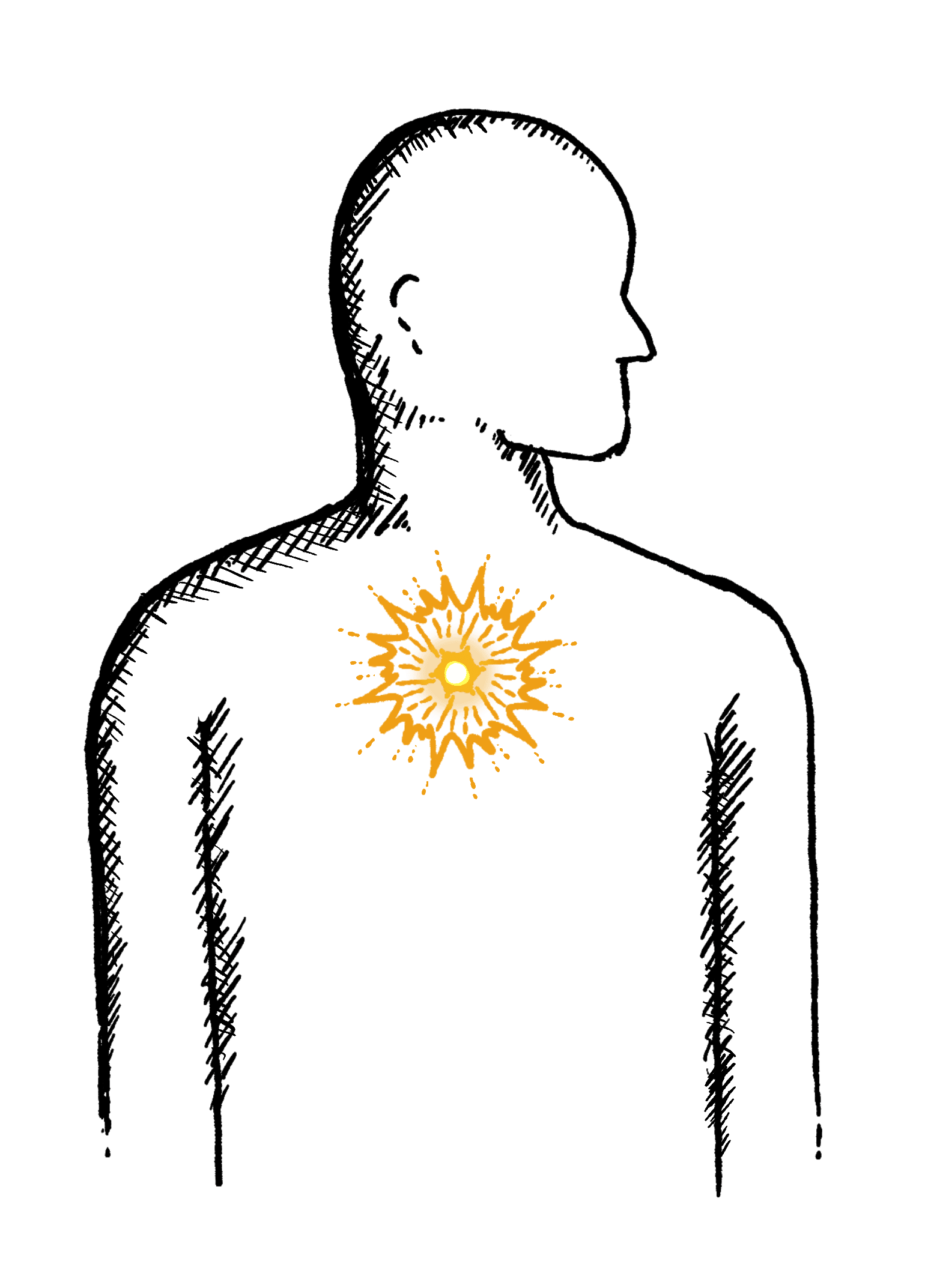
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
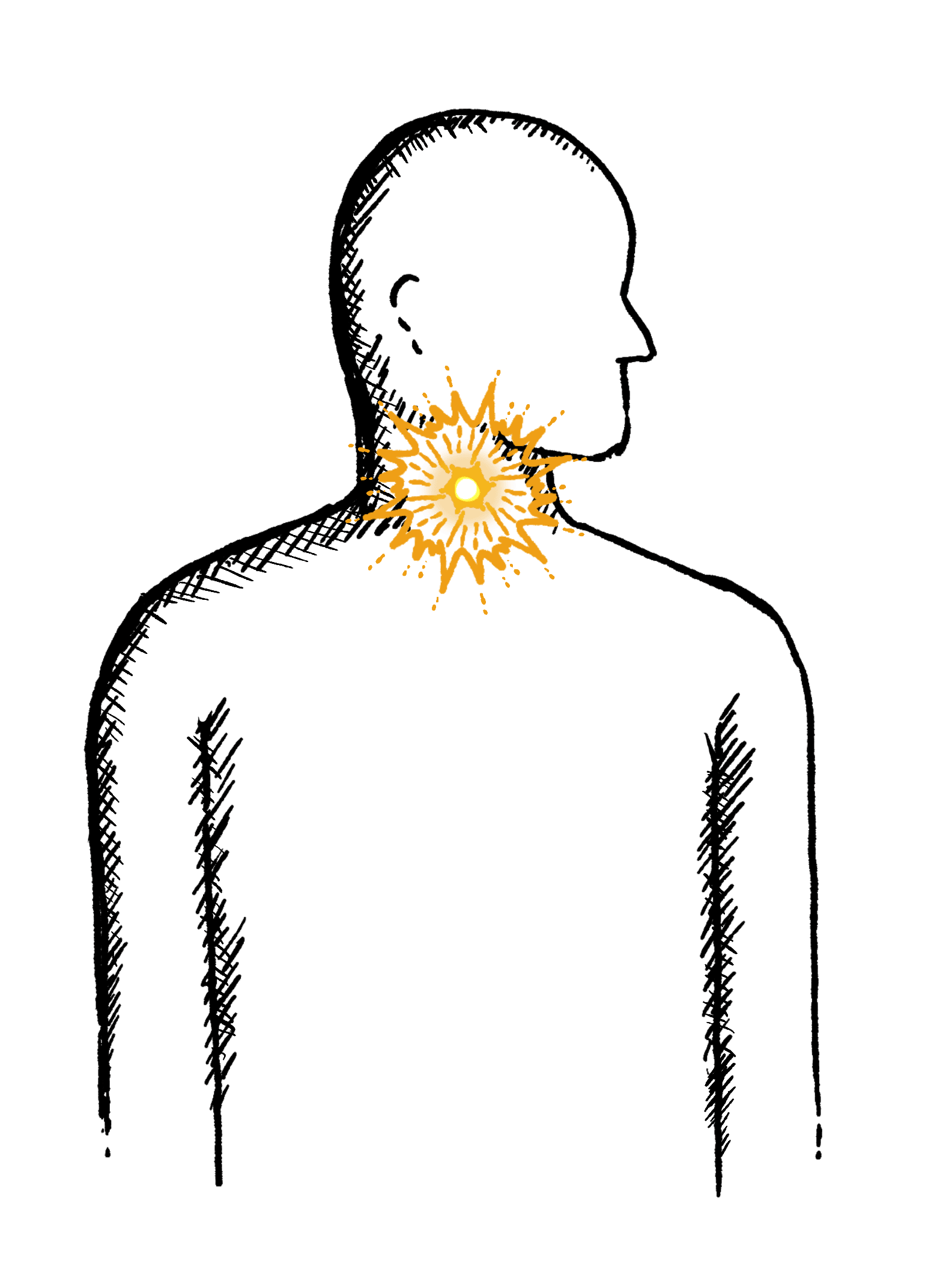
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
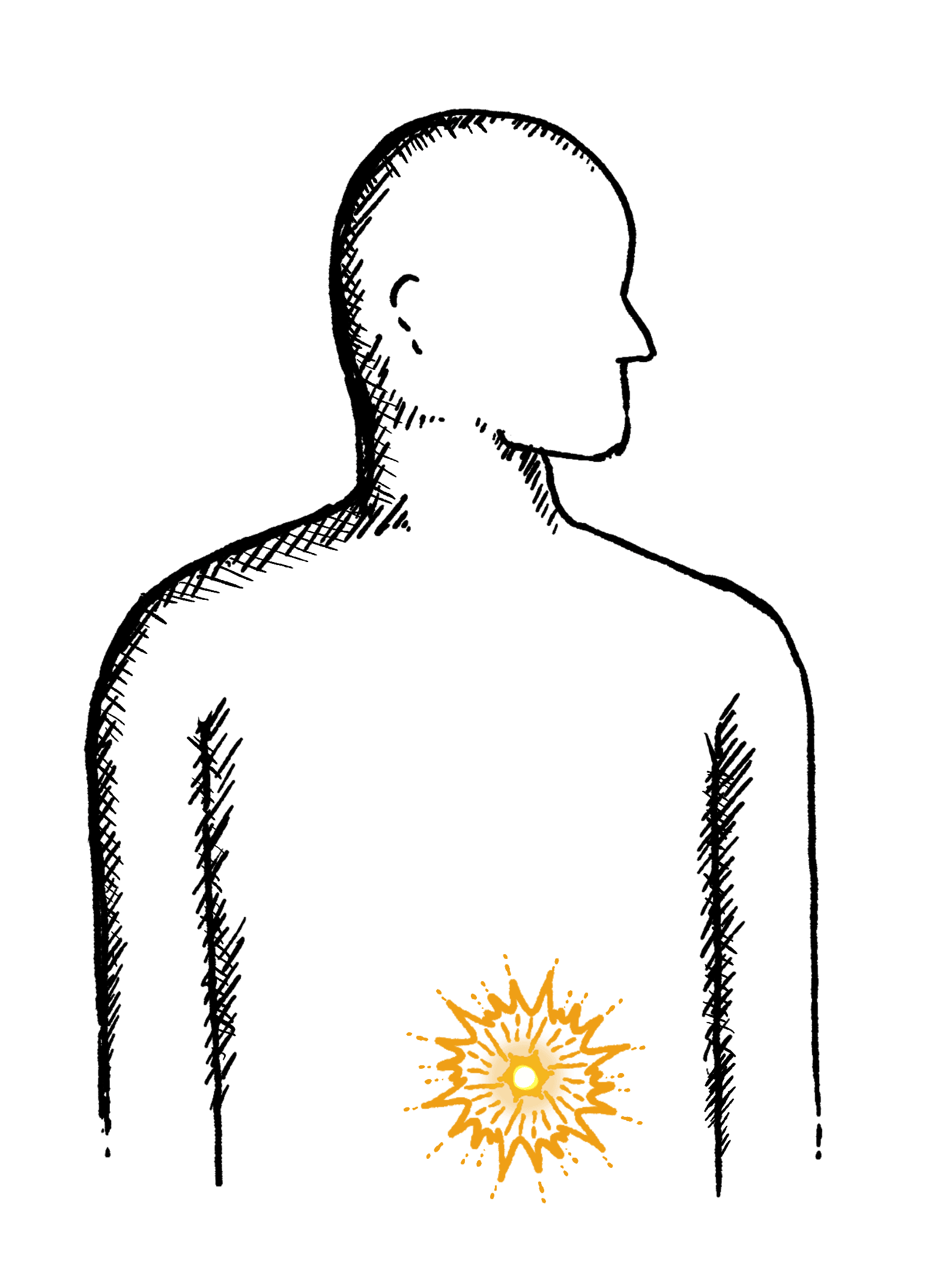
Diarrhoea
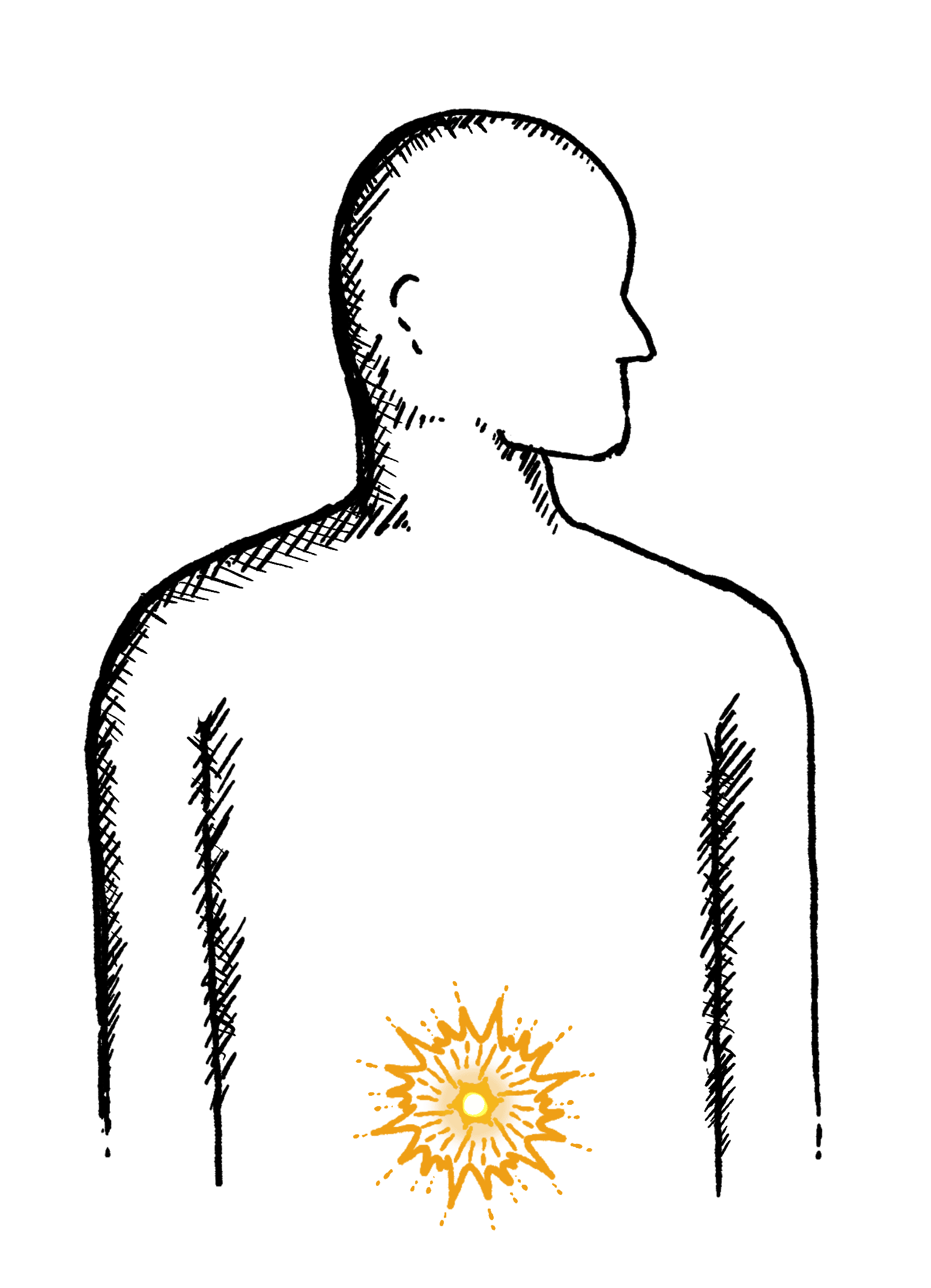
Loose or explosive stools, can’t get to a toilet in time
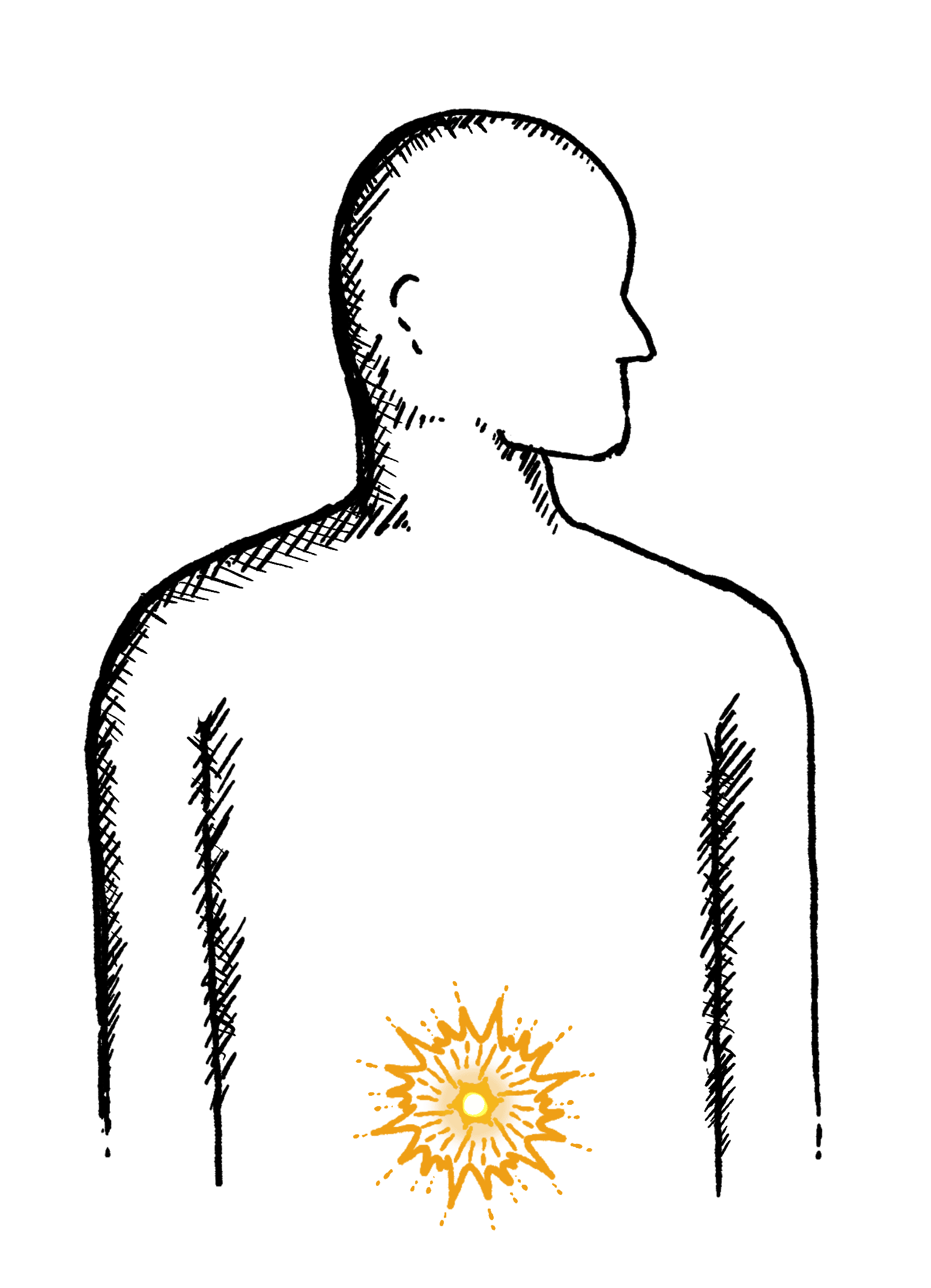
Abdominal Pain
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

