Understanding Faecal Microbiota Transplantation (FMT): What It Is and Why It Matters
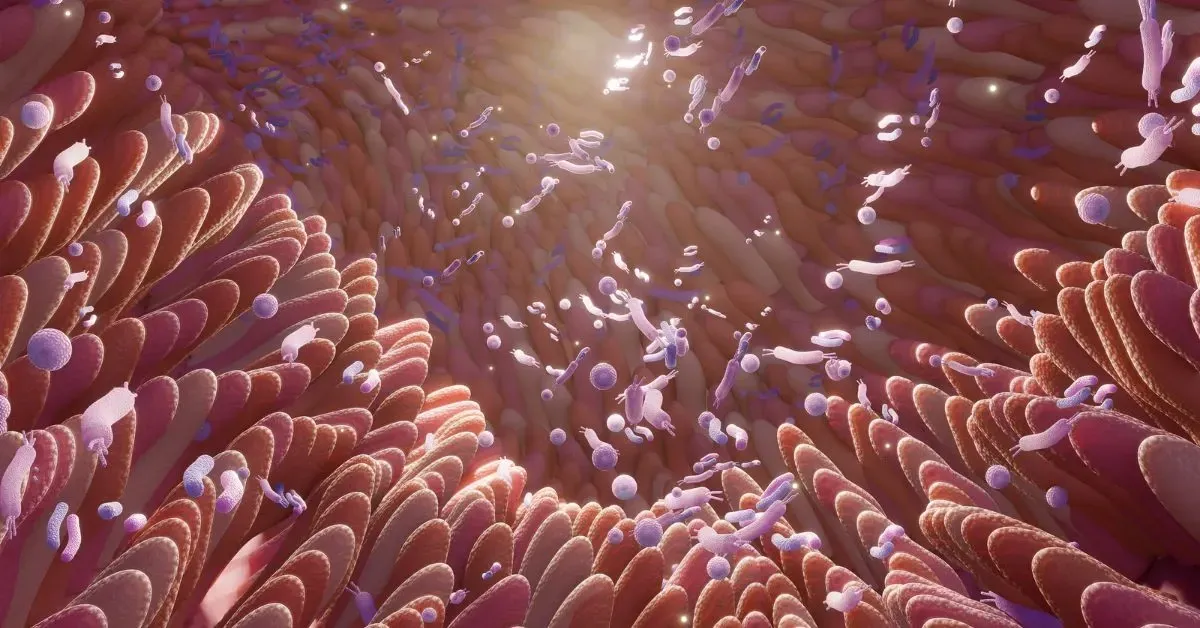
The gut is home to trillions of microorganisms, collectively known as the gut microbiota, that play a vital role in digestion, immunity and overall health. In recent years, scientists have begun exploring whether altering or restoring the balance of gut microbes could help in the treatment of various diseases.
One of the most discussed interventions in this space is Faecal Microbiota Transplantation (FMT). This involves transferring gut bacteria from a healthy donor to another individual, under medical supervision, within a controlled clinical setting.
This blog explores what FMT is, where it is currently used, what researchers are continuing to study and what this means for IBS patients.
Living with long-term IBS symptoms and looking to find out more about clinical support options? Request our factsheet (this will be shared with you via email) or get in touch with our team.
What is FMT?
Faecal Microbiota Transplantation (FMT) involves the transfer of processed faecal material from a healthy donor into the gastrointestinal tract of a recipient. The aim is to introduce a new, diverse microbial population into the gut. It is also referred to as Intestinal Microbiota Transfer (IMT).
While the concept might sound unusual, it reflects a growing recognition of the central role the microbiome plays in human health.
Where is FMT currently used?
Currently, FMT is approved for the treatment of recurrent or treatment-resistant Clostridioides difficile (C. difficile) infection. C. difficile is a bacterial infection that can cause severe diarrhoea and colitis and is often resistant to antibiotics. In cases where standard treatment fails, FMT has been shown in clinical trials to be effective in clearing the infection, with success rates of around 90% in some studies.
What is FMT being studied for?
FMT is being studied in a number of other medical conditions, primarily within research settings and structured clinical trials. Alternative routes of administration are also being studied.
Irritable Bowel Syndrome (IBS)
IBS affects around 1 in 10 people and is characterised by abdominal discomfort, bloating and changes in bowel habits. Research into FMT for IBS is showing emerging evidence that suggests a benefit in certain subtypes, mainly constipation-predominant IBS (IBS-C), while others show little or no effect overall. Researchers continue to explore whether microbiome-related therapies may help specific subgroups of IBS patients.
Exploring the Microbiome in IBS Support
If you are living with long-term IBS symptoms and would like to find out more about clinical support, we offer a structured assessment service through the Functional Gut Microbiome Clinic, request our IBS Support Factsheet here.
NEW STUDY
At the Functional Gut Clinic, we are at the forefront of not only conducting this essential research, but also translating the findings into carefully controlled, evidence-led treatment programmes for patients. Our TrIuMPH study was a randomised, double blind, placebo controlled, phase II trial assessing the safety and efficacy of an IMT product in patients with IBS-C. Read more about our clinical trial here.
Inflammatory Bowel Disease (IBD)
FMT is also being studied in ulcerative colitis, a type of IBD affecting the colon. Some trials suggest it may help reduce inflammation and support remission, although results vary and more long-term data are needed.
Metabolic Conditions
Conditions such as metabolic syndrome, which includes obesity, insulin resistance and high blood pressure, have also been linked to changes in the gut microbiota. Some early-stage studies have explored FMT’s potential to influence metabolic markers, although any benefits seen so far appear to be temporary.
Neurological and Immune Conditions
There is growing scientific interest in the gut–brain–immune connection. FMT has been explored in early research relating to autism spectrum disorder and Parkinson’s disease, as well as in cancer patients undergoing immunotherapy, where the gut microbiota may influence treatment response. These areas remain investigational.
Is FMT safe?
In clinical studies, FMT is generally well tolerated. Mild side effects such as temporary bloating, discomfort, or diarrhoea are the most commonly reported. Rare but serious risks, such as infection, have also been documented, which is why FMT must always be performed under strict clinical supervision, using rigorously screened donor material.
FMT is not suitable for everyone, and patients with complex medical histories are typically assessed in detail before any consideration is given to this kind of intervention.
The future of FMT research
FMT continues to be the focus of active clinical research, particularly in relation to chronic gastrointestinal disorders, including IBS-C. Researchers are also working to understand which patient characteristics (such as gut microbiota composition, symptom patterns, or prior treatments) may influence who is most likely to benefit.
Importantly, the use of FMT for conditions beyond C. difficile infection is not routinely available and remains unlicensed. Any future use in these areas must be based on robust clinical trials and regulatory review.
Supporting patients with IBS
If you are living with long-term IBS symptoms and are curious about microbiome-related testing or clinical pathways, we offer a structured assessment service through the Functional Gut Microbiome Clinic.
If you're interested in finding out more about the role of the microbiome in IBS, and whether clinical support could be appropriate, request our factsheet to be shared via email. Or alternatively, contact our team to discuss your options.
Disclaimer: This article is intended for educational purposes only and does not constitute medical advice or offer of treatment. FMT is only licensed for treatment of recurrent C. difficile infection. Use in other conditions remains investigational. By requesting further information, you confirm that this is an unsolicited patient-led enquiry. Patients should always seek professional medical advice before considering any treatment.

