Bloating
Struggling with bloating? Here’s what you need to know to find relief.
ALL TEST ARE ACCREDITED & REGULATED BY


What is bloating?
When you’re bloated, your stomach or abdomen can feel full and uncomfortable, or even painful.
This bloating happens when your gastrointestinal tract contains too much gas or air. Bloating can be mild, or more severe, and may present as:
– A visibly distended or swollen abdomen
– Feeling very full and uncomfortable
– Feeling of tightness in the abdomen
– Excess gas – belching and/or flatulence
– Rumbling or gurgling
There are several causes of bloating, so it’s important to diagnose the cause of your bloating and find out why it’s happening to you.

Why does bloating happen?
Prolonged periods of bloating could indicate an underlying health problem, if so you should see your GP.
Possible causes can include:
Irritable bowel syndrome (IBS diagnosis)
Ulcerative colitis, a form of inflammatory bowel disease (IBD), where the inner lining of the large bowel is inflamed and develops ulcers
Crohn’s disease, the other form of IBD, where some parts of your colon are inflamed
Too much bacteria in your small intestine (called small intestinal bacterial overgrowth, or SIBO)
Gastroesophageal reflux disease
Food intolerances, especially lactose or fructose intolerance
Producing too much gas (dysbiosis and fermentation)
Weight gain
Stress or anxiety
Delays in your food and drink moving on from your stomach (called gastroparesis)
Eating too quickly, so that you swallow too much air (called aerophagia)


Diagnosing bloating
Feeling bloated is no fun, but once you know what’s going on you can start to manage your symptoms and the underlying causes.
Testing options:
At the Functional Gut Clinic, we can run the following tests to diagnose the causes of bloating:
Gastric emptying test– which measures how quickly food leaves your stomach
Carbohydrate malabsorption breath test– which finds out if you have certain food intolerances (lactose or fructose)
Small intestinal bacterial overgrowth (SIBO) breath test– which finds out if you have an overgrowth of bacteria in your small intestine (called SIBO)
Oesophageal manometry– which measures the function of your oesophagus (food pipe)
24-hour pH impedance monitoring– which looks at whether you have any reflux
Colonic transit study-a non-invasive test which looks at how long it takes for faeces to pass through your bowl
Learn more about bloating

What Is Gastroscopy? And Why Is It Needed?
A gastroscopy involves threading a small tube with a camera down your food pipe (oesophagus) and into your stomach to look for any abnormalities. Common reasons for a gastroscopy include acid reflux, difficulty swallowing, and stomach pain. The procedure is a little uncomfortable but otherwise safe.
Otherwise known as an “endoscopy,” the procedure allows your doctor to see problems within your body without making an incision. The camera is threaded via your mouth. If necessary, the doctor will take small biopsies during the procedure for later analysis.
What Is a Gastroscopy?
Gastroscopy is a diagnostic medical procedure where a doctor or nurse views your stomach using an endoscope (a thin tube with a camera and light on the end). This device is about as thick as your little finger.
Numbing gel is often used at the back of the throat to make the procedure more comfortable. You can also be sedated if you wish. The camera is inserted through the mouth, into the oesophagus, and down to the stomach and sometimes the duodenum (the first part of the intestines).
The procedure allows the doctor to spot and record any abnormalities in the food pipe, stomach, and duodenum for later analysis. The doctor may also take a biopsy if they find an area that looks abnormal. The procedure is sometimes known as an “upper GI endoscopy” or “OGD.”
Why You Might Need a Gastroscopy
Your doctor may suggest a gastroscopy if there are signs that something isn’t quite right in your oesophagus, stomach, or upper small intestine. It’s often used to investigate ongoing problems such as:
Frequent heartburn or acid reflux
Difficulty or discomfort when swallowing
Ongoing upper tummy pain
Unexplained sickness or vomiting
Losing weight without trying
Possible internal bleeding (for example, vomiting blood or passing black stools)
Indigestion that isn’t improving with treatment
A gastroscopy can also be used to keep an eye on pre-existing conditions like Barrett’s oesophagus, stomach ulcers, or coeliac disease. It gives your doctor a clear view of what’s going on inside and helps them decide the best way to treat it.
What Happens During a Gastroscopy?
Gastroscopy is almost always an outpatient procedure. That means you arrive that day, undergo the procedure, and then head home. It’s advised that you organise a ride home, especially if you choose to be sedated, as the sedative means you cannot drive safely.
The doctor or nurse will ask you to lie on your side. A plastic mouth guard is placed between your teeth to prevent you from biting the endoscope. It is then threaded into your mouth and down into the stomach. It can be a little uncomfortable at first.
Your doctor will visualise your oesophagus, stomach, and duodenum via a monitor. Air is passed into the stomach to make it easier to see. This can cause bloating and belching — don’t be embarrassed; this is completely normal.
If the doctor identifies anything unusual, they’ll take a painless biopsy. It’ll be sent to a lab for testing. This doesn’t mean anything is wrong.
Preparing for a Gastroscopy
You will receive instructions from the hospital or outpatient department before your procedure. The typical preparations are:
Avoid eating or drinking for 4-6 hours before the procedure
Stop certain medications before the procedure
Ask someone you trust to accompany you home if you have the sedative
Once the procedure is completed, you cannot drink alcohol or operate machinery for 24 hours due to the sedative. Always wait for the effects to wear off. If you only have the anaesthetic throat spray (numbing spray), you can carry on as normal.
Complications of a Gastroscopy
A gastroscopy is a safe procedure. Tens of thousands of patients undergo a gastroscopy annually without any complications. However, like any medical intervention, it carries some risks.
The most common complications include:
Abdominal pain. If it worsens or becomes severe, seek medical attention
Fever. A raised temperature can indicate infection.
Difficulty breathing
Vomiting blood
In extreme cases, you can develop a chest infection or pneumonia. However, most people just feel a little tired and have a sore throat for a few days afterwards.
Get to the Root of Your Heartburn Causes
A gastroscopy is a common first-line investigation for prolonged heartburn and gastroesophageal reflux disease. It can identify the underlying causes behind your symptoms, especially if they haven’t improved with medications like proton pump inhibitors.
Don’t struggle with acid reflux — we can help you diagnose the problem.
If you’re struggling with ongoing reflux or indigestion, finding the exact trigger can make all the difference. The Functional Gut Clinic offers specialist testing to get to the root of common heartburn causes and other digestive symptoms, so you can move beyond guesswork and start a treatment plan that works.
Hear from people we’ve helped, just like you.
"Very professional while welcoming and friendly"
"The manner and demeanour of all staff from reception to people carrying out the test was very professional but welcoming and friendly. Atmosphere is very relaxed and all instructions clear and concise."
London Patient

"Highly recommend this"
"Thanks to Dr Hobson and everyone at the Functional Gut Clinic. The whole team is very kind and generous and they are doing things that are cutting edge and they actually get results."
Manchester Patient

"Highly recommend this"
"After stopping my lansoprazole, every time I had a warm drink, I could feel it burn all the way down to my stomach. Thank you to Sam for making me feel at ease." - Manchester Patient

"My experience could not be better"
"Pleasant and knowledgeable staff that made the experience more enjoyable than it should be!" - London Patient

"Very friendly and knowledgeable"
"An excellent service from beginning to end. I would recommend to anyone who was considering having testing done. Very friendly and knowledgeable!" - Manchester Patient

"Very kind and helpful"
"It was also great to have time to talk to the clinicians – very important when you have problems. Reception staff also very kind and helpful." - Manchester Patient

Are you experiencing any other symptoms
Symptoms are often closely connected. Find out more below.
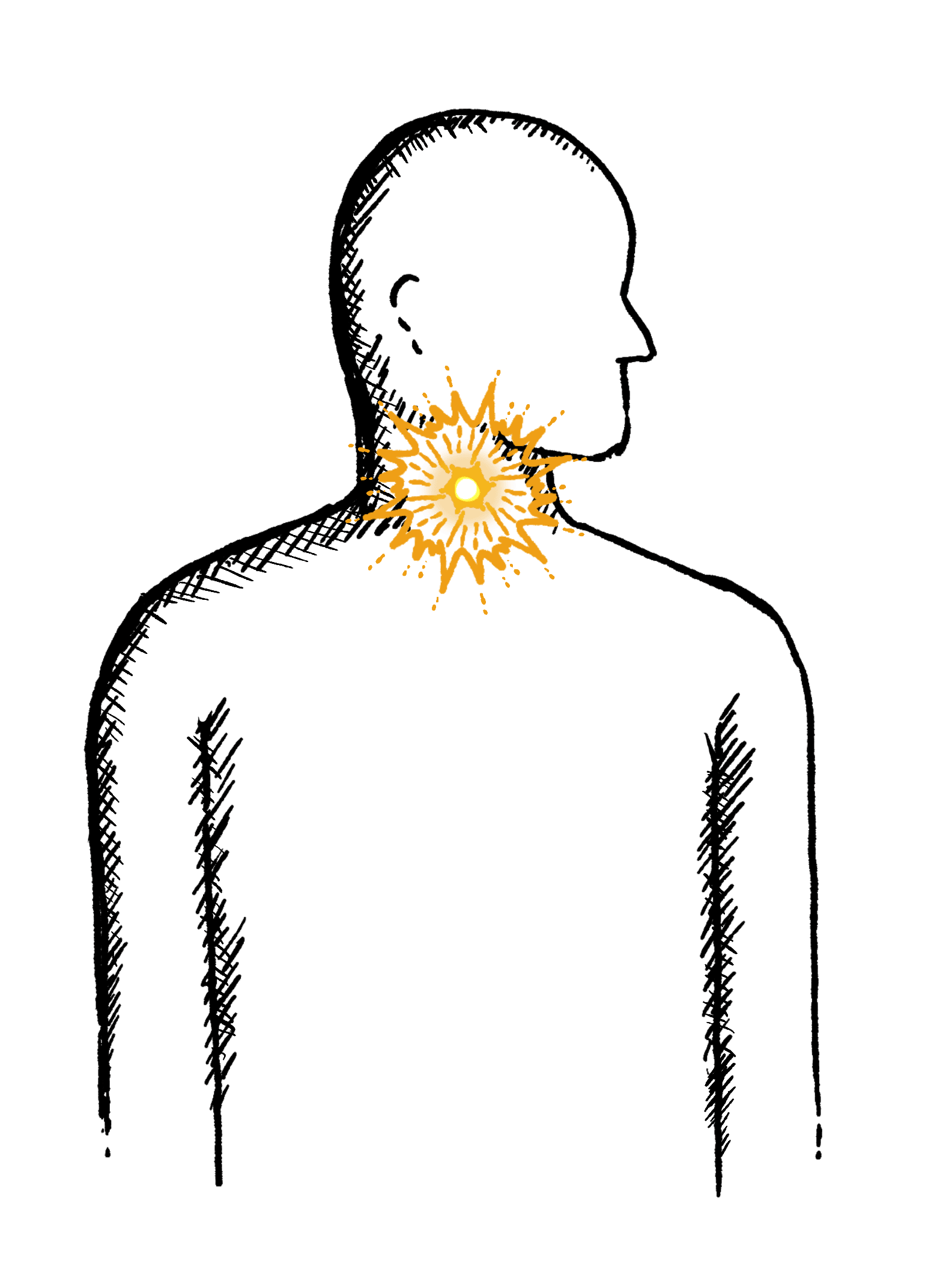
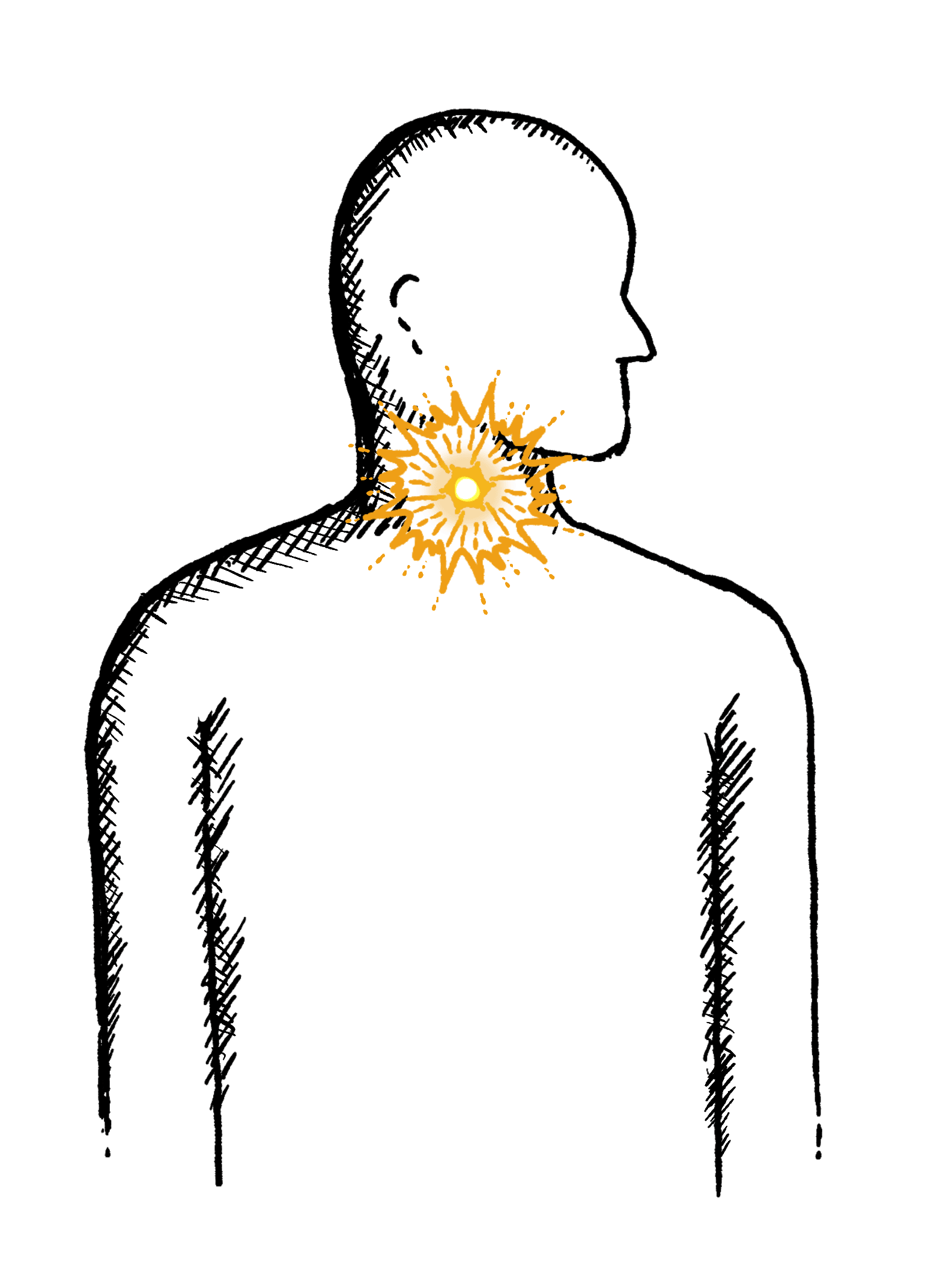
Reflux
Burning mid-chest, worse when bending or lying down
Constipation
Difficulty going to the toilet, unusual stools, often with stomach ache or intestinal cramps, bloating, nausea or appetite loss
Heartburn
A burning pain in your chest, just behind your breastbone.
The pain is often worse after eating...
Regurgitation
Bringing food or drink back up, difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Swallowing Issues
Dysphagia - difficulty swallowing, feeling that food or drink is stuck in your throat, horrible taste in your mouth
Diarrhoea
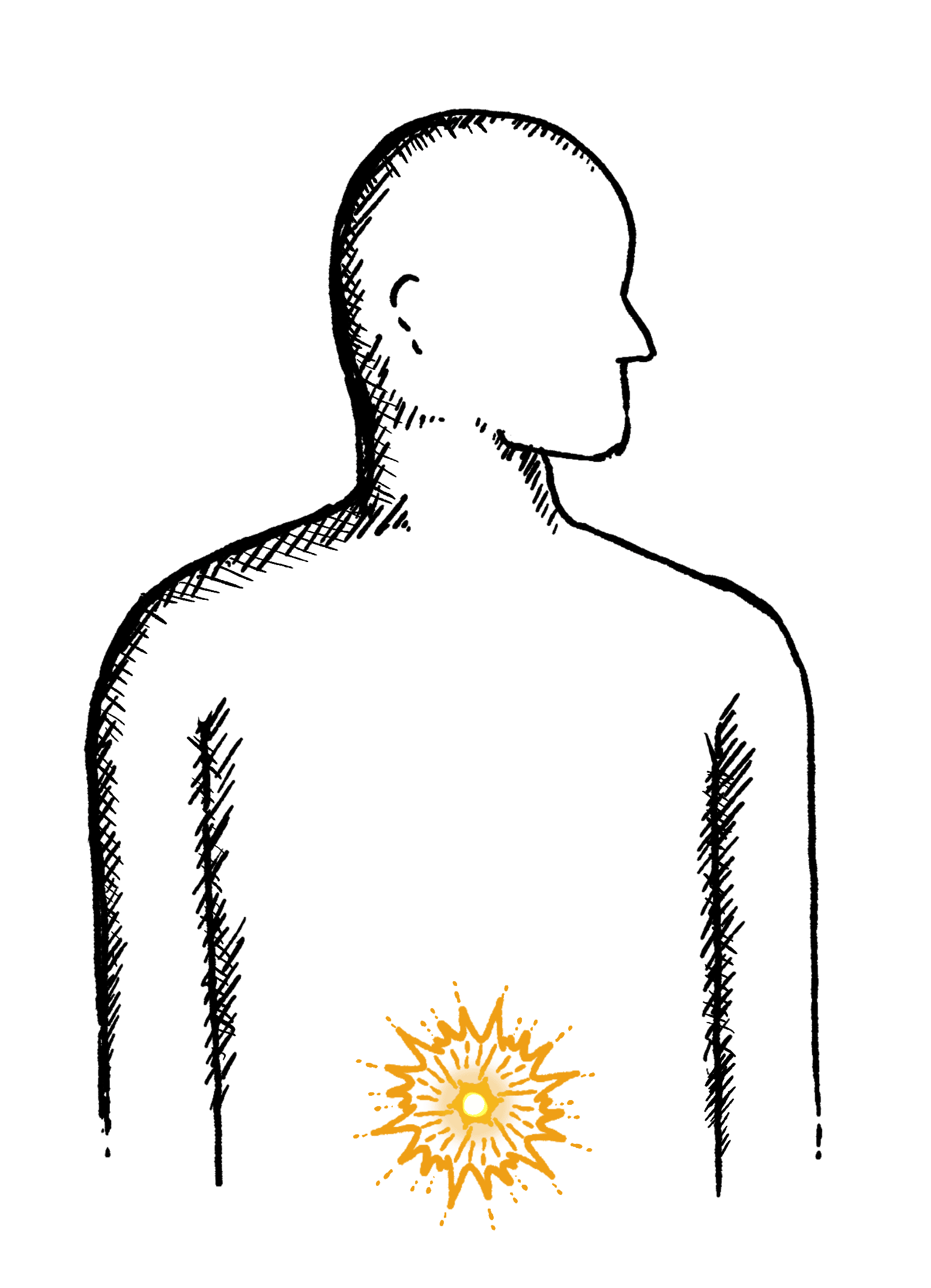
Loose or explosive stools, can’t get to a toilet in time
Abdominal Pain
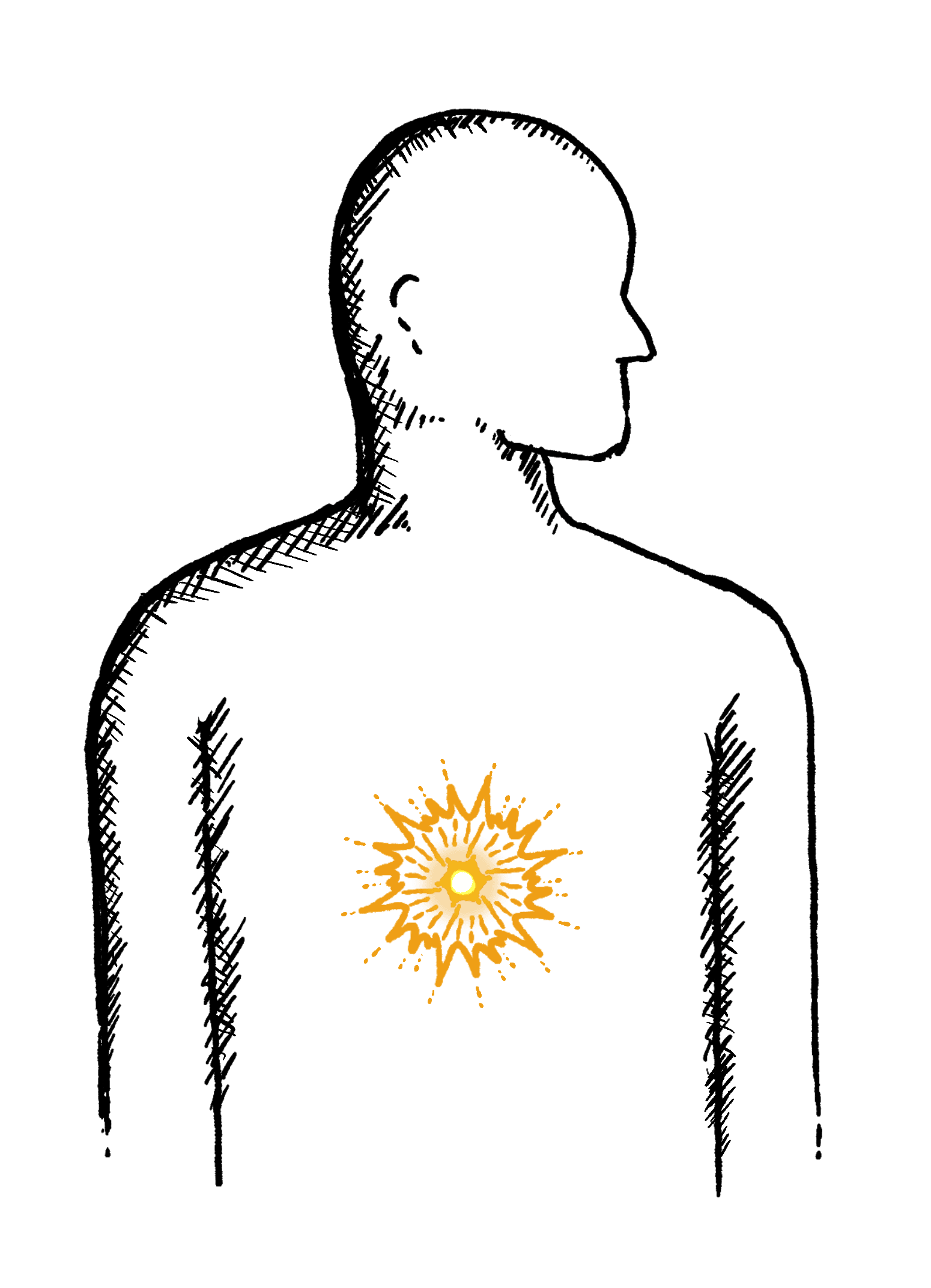
Cramps; sharp or dull pain, Bloating, Excessive belching, Nausea or vomiting
Faecal Incontinence
Stools leak unexpectedly, Can’t get to a toilet in time
IBS
Abdominal pain or cramping, bloating, changes in bowel habits and urgency, gas

